Get Complete Project Material File(s) Now! »
MALE FACTOR IN REPRODUCTION
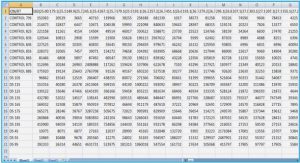
Human semen is produced as a concentrated suspension of spermatozoa stored in the paired epididymides. During ejaculation it is mixed with, and diluted by, fluid secretions from the accessory sex organs. It is present as a fluid conglomerate emitted in several boluses. Semen has two major quantifiable attributes: (1) the total number of spermatozoa reflecting sperm production by the testes and the potency of the post-testicular duct system, (2) the total fluid volume reflecting the secretory activity of the glands. Semen reflects a heterogeneous cell suspension that differs among individuals in protein content, sperm number, pH, volume etc. These factors defined by the World Health Organization (WHO) are crucial when judging semen quality. Semen quality (Tab. 1, 2) is taken into account to measure male fertility in clinical andrology, male fertility, reproductive toxicology, epidemiology and pregnancy risk assessments (WHO, 2010). The quality of semen is verified by the presence of several components. For instance, the abundance of proteolytic fragments, decreased seminal level of albumin, poor testicular contribution characterize the oligozoospermic ejaculates. Seminal glycoprotein deficiency, the increased level of acid phosphatase and increased prostatic secretory activity are associated with asthenozoospermia (Autiero et al., 1991). Since specific substances can be assigned to specific reproductive compartments, chemical substances serve as diagnostic markers. Neutral -glucosidase, carnitine, glycerolphosphocholine represent the indicators of epididymal functions. Prostate function is evaluated according to the levels of fructose, prostaglandins, citrate, zinc and prostatic acid phosphatase (Rowe et al., 1993). Semen also contains several immunoregulatory factors as well as immunogenic agents that represent the possible targets of activated inflammatory cytokines, leukocytes and complement cascade in any part of the female genital tract (Chung et al., 1994; Sharkey et al., 2007; Rodriguez-Martinez et al., 2011). One of the most common devices to evaluate spermiogram is the Makler counting chamber. It is composed of a metallic base unit, semi-circular ring, cover glass with surface graticule (Fig. 1, Makler, 1980).
The inability to achieve penile erection or to maintain an erection until ejaculation, caused by the congenital, neurological and metabolic disorders or abnormalities, is known as erectile dysfunction (impotentia coeundi). In addition, if spermatogenesis is disrupted, it results in the inability to procreate (impotentia generandi) (Ulcova-Gallova, 2006).
Seminal fluid
Seminal fluid (SF), also cited as seminal plasma, represents a part of the semen containing a range of organic/inorganic substances (e.g. neutral α-glucosidase, hyaluronidase, carnitine, glycerolphosphocholin, fructose, prostaglandins, citrate, zinc, selenium) that are necessary for the physiological metabolism of sperm. The seminal complex mixture of secretions originates in the testis, epididymis and accessory glands including the prostate, seminal vesicles and Cowper‟s gland. It also acts as a nutritive, transport and buffering medium of pH 7.35 – 7.5 that defines the main SF functions: sperm protection from the acidic environment of the vagina, metabolic support and competence, liquefaction and clot formation. SF composition is similar to blood plasma. However, it differs in saccharide content (Kumar et al., 2009; Rodriguez-Martinez et al., 2011; Brazdova et al., 2012a).
Semen liquefaction is caused by the fibrinolytic activity of some proteinases and peptidases present in prostatic SF. The key role of seminal enzymes (kallikrein-like protease 3, prostate-specific antigen) consists of a clot digestion formed immediately after ejaculation. It is said that SF containes hundreds of proteins of molecular or catalytic activity including additional proteins classified as their regulators (Yousef and Diamandis, 2001; Pilch and Mann, 2006).
In general, seminal proteins can be divided into three different groups. The first group contains the extracellular and intracellular proteins supporting basic SF function. The second group, originating in proteasomes and membrane-enclosed structures, is mainly involved in oocyte-sperm fusion. The third group is known as the potential biomarkers of testis/prostate cancer and male infertility as they represent the abraded epithelial cells from tissue surface (Pilch and Mann, 2006).
SF is in routine examined to evaluate pathological spermiogram and to monitor the progression of either testis or prostate cancer. In particular, prostate cancer is diagnosed by the seminal level of prostate-specific antigen (PSA), prostatic acid phosphatase (PAP), prostate stem-cell antigen or glutamate carboxypeptidase II that is a prostate-specific membrane antigen (Jones, 1991; Ostrowski and Kuciel, 1994; Cao et al., 2003). Prostate cancer can be diagnosed by the serum PSA level. The serum concentration of 4 ng/ml means a 20-30% risk of prostate cancer. The risk increases approximately to 60% with a PSA level higher than 10 ng/ml (Fung et al., 2004). An early elevated level of serum zinc alpha-2-glycoproteins (ZAG), originally secreted by the prostate, indicates tumor growth as well. PSA, PAP and prostate-specific protein-94 (PSP-94) belong to the prostate secretion that accounts for about 30% of the total SF volume. This SF fraction is in direct contact with sperm and is the first to confront the cervical tissues. PSA ( -seminoprotein, seminin, kallikrein-3, P30 antigen, semenogelase) is a 33 kDa member of the glandular kallikrein subfamily of serine proteases. In particular, it is a member of the kallikrein subgroup of the (chymo)-trypsin serine protease family. It differs from the prototype member of this subgroup, tissue kallikrein, by possessing specificity more similar to that of chymotrypsin than trypsin. PSA is known as a zinc-binder and the most common protease in human semen. It is mainly released in proteasomes. It hydrolyzes semenogelin-1, thus leading to the liquefaction of the seminal coagulum. Its activity is strongly inhibited by zinc ions. This inhibition is relieved by exposure to semenogelins, which are avid zinc binders (Espana et al., 1991; Utleg et al., 2003; Pilch and Mann, 2006). PAP belongs to histidine acid phosphatase family, is stored in lysosomes and has an acid pH optimum below 7.0. It is a non-specific tyrosine phosphatase that dephosphorylates macromolecules and inactivates lysophosphatidic acid in SF. Its isoform 2 acts as a tumor suppressor of prostate cancer through the deactivation of mitogen-activated protein kinases. Decreased PAP level exhibits poor liquefaction (Autiero et al., 1991; Tanaka et al., 2004).
It contains the membrane-enveloped secretory vesicles. The fructose level is a marker of seminal vesicle function. High concentration of fructose is essential for sperm survival in the female reproductive tract. Fructose and other sugars are a source of energy for mitochondria-rich sperm. A decreased fructose level means a lower intensity of fructose oxidation. It leads to a lactate accumulation, which results in reduced sperm motility (Anderson et al., 2004). SF is rich in proteins secreted by seminal vesicles. Semenogelin I and II, fibronectin and fibronectin-related derivates belong to the gel-forming proteins. They are active after the cleavage by kallikrein-like protease and then have a role in entrapping sperm into a viscous gel immediately after ejaculation. They are also involved in sperm capacitation and sperm-oocyte interaction. Another SF element is lactoferrin, thanks to which SF may have an antimicrobial activity. SF content also involves albumin, serum and testis derived, that is a predominant protein participating in cholesterol removal from the sperm membrane during capacitation. The decreased seminal level of albumin and the increased seminal level of cholesterol are found in oligozoospermic men (Lilja et al., 1987; Autiero et al., 1991; Kosanovic and Jankovic, 2010).
Seminal components that bind to the acrosomal sperm head region protect sperm and are then carried together with it into the higher female genital tract. SF plays an important role in moving the sperm into the female reproductive tract due to its high content of transforming growth factor beta (TGF ) and prostaglandin E (PGE), both of which inhibit the function of natural killer (NK) cells and neutrophils that are recruited into the superficial epithelial layers of the cervical tissues. SF is rich in PGE of 19-hydroxy form that promotes an expression of chemotactic interleukin 8 (IL-8). TGF is synthesized in the prostate and is testosterone-dependent. This glycoprotein belongs to cell-secreted molecules and occurs in 75% in the latent form in SF. It is further activated in the female reproductive tract by either the enzymes of male/female origin, acidic vaginal pH or through conformational change after an interaction with epithelial cells. The remaining proportion of TGF , β5%, exists in an active form (Denison et al., 1999; Robertson et al., 2002). TGF acting may result in the immune tolerance of seminal antigens, for which TGF I is, most likely, responsible. It is a cytokine of TGF family. A divergent member of this family is growth/differentiation factor 15 (GDF 15), which is highly abundant in SF. Surprisingly, its level is not related to semen quality but its expression serves as a cancer marker, often in combination with PSA. However, GDF 15 has antitumorigenic activity. In contrast, the high level of GDF 15 in female serum corresponds to spontaneous abortion as it is expressed in placenta as well. It has been suggested that thanks to the presence of seminal antigens on a conceptus, TGF facilitates the female immune tolerance to a fetus (Robertson, 2005; Soucek et al., 2010).
SF includes a repertoire of signaling molecules interacting with epithelium in the female reproductive tract. SF may modulate the chemotactic and phagocytic response of the female reproductive tract. Phagocytes serve to filter out the morphologically abnormal sperm. Sperm selection is based on morphological or antigenic structures. Mainly, the immune modulating properties are mediated by the prostaglandins of the E series, complement inhibitors, cytokines and proteins capable to bind IgG antibodies (Tomlinson et al., 1992; Kelly and Critchley, 1997). Local reactions may lead to an inflammation (Robertson, 2005).
However, SF has a built-in mechanism preventing an immunological sensitization of the female against sperm as well as seminal structures. This protective system exists due to the presence of immune inhibitors originating in the male sex accessory glands (Prakash, 1981). SF has been suggested to be the modulator of sperm-induced inflammation that leads to sperm elimination from the female genital tract (Troedsson et al., 2005).
SF elicits endometrial changes by inducing pro-inflammatory cytokines and cyclooxygenase-2. Their presence leads to macrophage and dendritic cell recruitment into the female reproductive tract. Seminal components activate the income of neutrophils into the endometrial stroma (Robertson, 2005; Bronson, 2011; Morrell et al., 2012). However, it has been proved that the influx of neutrophils is higher and faster when the washed sperm inseminated (Rozeboom et al., 1999). This fact proves the protective and signaling activity of SF. The immuno-suppressive activity prevents the iso-immunization of the female reproductive tract and suppresses the cell-mediated cytotoxicity (Lord et al., 1977). Seminal prostaglandin D2 is known for its immuno-suppressive effect, by which the anti-sperm antibody formation is avoided in the female genital tract. The immuno-modulating properties are mediated by prostaglandin E, complement inhibitors, cytokines and proteins capable of binding the Fc region of IgG. These IgG-binding proteins are Fc receptor-like proteins. In general, seminal antibody-binding proteins contribute to sperm protection against immune-mediated damage by enabling successful sperm passage in the female reproductive tract and by blocking an interaction with immune effectors. For instance, prolactin-inducible protein (PIP), which is a secretory glycoprotein located in seminal vesicles, binds to immunoglobulin G via its Fc fragment, it may therefore be involved in immune regulation by trapping anti-sperm antibodies (ASA) and neutralizing them (Chiu and Chamley, 2002; Chiu and Chamley, 2003).
SF has been considered to be linked to the IgE-mediated rare reaction to semen (Weidinger et al., 2006). This rare phenomenon was firstly reported by James (1945). Human seminal plasma allergy (HSPA) or the so-called hypersensitivity to semen is defined by localized and/or systemic symptoms after exposure to seminal fluid. The symptoms occur immediately after contact with semen or even within several hours after intercourse. The local symptoms include vulvar/vaginal itching, burning, redness and swelling. Local reaction can appear on any semen contact site. Local symptoms can be misdiagnosed as chronic vulvo-vaginitis caused by bacteria, yeasts, viruses and other parasites. Systemic features include generalized urticaria, angioedema (face, tongue, lips, throat), dyspnea, wheezing, cough, chest tightness, rhinorrhea, nausea, vomiting, diarrhea. Generalized malaise may result in an anaphylactic shock, which is a life-threatening reaction. The symptoms can manifest after the first time intercourse in up to 50% of cases. Response mediated by IgE antibodies is then the most common mechanism. It has been suggested (Basagana et al., 2008) that female patients experiencing any allergic symptoms after/during the first time intercourse might be sensitive to other antigens/allergens that cross-react with SF. Basagana et al. (2008) has already proved the IgE cross-reactivity among proteins from dog epithelium and PSA. Patients diagnosed with HSPA have difficulties conceiving but infertility has not been demonstrated, so far (Shah and Panjabi, 2004; Weidinger et al., 2006; Bernstein, 2011).
Spermatozoa
Mature male gamete is commonly known and cited as sperm but specifically called as spermatozoa. It was firstly described in 1677 by Anthony van Leeuwenhoek. Sperm is a male reproductive cell of approximately 55-65 µm, containing genetic information and participating in the fertilization of an ovum (150-300 µm). Sperm consists of a head, middle section (mid-piece) and tail (Fig. 2). It is characterized by a minimum of cytoplasm. The head contains a nucleus, its shape is flat and oval in order to attach and easily penetrate an oocyte. An anterior peak of sperm head carries a cap-like structure called acrosome. It is designed, thanks to its hydrolytic enzymes, to help the sperm to penetrate the oocyte. The middle section consists of mitochondrial spiral, outer dense fibers and core microtubular structures. The mitochondrial formation contains the enzymes of oxidative phosphorylation. The mid-piece is, therefore, composed of substances that propel the tail. The tail enables the sperm to be motile by rotating in a circular motion, not from side to side like a whip (Collins discovery encyclopedia, 2005). The speed of sperm in ejaculate ranges from 10 to 60 µm/s. Its movement is based on the enzymatic and microtubule components, and is calcium and magnesium dependent. The tail is able to move ten times per second. Twenty thousand movements are estimated to be needed to reach the oocyte. In vitro, the speed is positively influenced by methylxanthins, lower temperature, and negatively by proteolytic enzymes, hydrogen peroxide and human saliva as it contains amylase and lysozyme enzymes (Ulcova-Gallova, 2006).
Normal sperm is characterized by an oval head with a long tail. Abnormal sperm has the defects of any body part (Fig. 3). Defects occurring on the head cause different shapes: large (giant), small (micro), elongated, irregular, amorphous, and then involve the acrosome deficiency and the so-called bicephalic head. The defective mid-piece is asymmetric, bent, thin, thick, irregular or with cytoplasmic droplets. The defective tail is coiled, shortened, hairpined, broken, duplicated or with terminal droplets. Any defects may impair the ability of the sperm to reach and fertilize the oocyte. In general, sperm morphological abnormalities are related to congenital background, varicocele, high fever, infection or drug use (Gilbert, 2000).
Spermatogenesis
Spermatogenesis (Fig. 4) is a complex process creating functional sperm, starting at puberty and ending with death. It occurs in the testis, progresses to the epididymis and takes approximately 64 days for completion. Effective maturation is conditioned by temperature, 2 °C lower than body temperature. This explains its location in external genitals. Sperm cells are then stored in the epididymides. The entire process is regulated by hormones (follicle stimulating hormone, luteinizing hormone, testosterone). It consists of three major steps:
(1) the multiplication of spermatogonia by mitosis, (2) meiosis to reduce the chromosome number from diploid to haploid, (3) the successful transformation of the round spermatid into the so-called spermatozoa. The spermatogonial population is created from the germ cells in the testis. The population then fuses with the Sertoli cells by creating seminiferous cords. After multiplication, several types of spermatogonia are distinguished: type A and B. The subsequent meiosis reduces the chromosome number from a diploid to a haploid form of type B spermatogonia. Type A diploid spermatogonium divides into two diploid cells called primary spermatocytes. The newly developed cells migrate into seminiferous tubules to undergo the meiosis by creating the secondary spermatocytes. The secondary spermatocytes are haploid. The next step reflects the forming of rounded spermatids. The differentiated spermatids mature in the epididymis into functional spermatozoa. There is an evidence of post-translational modifications that are considered to be essential for efficient spermatozoa. Some of them can activate capacitation directly in the epididymis or post-ejaculatory in the female reproductive tract. The cascade of modifications includes phosphorylation, glycosylation, proteolytic cleavage and methylation. A healthy man is usually able to produce up to 100 million of sperm/day. However, the concentration of 20 million/ml reflects, nowadays, the mean amount (Ulcova-Gallova, 2006; Warwick, 2006; Vacek, 2006; du Plessis et al., 2011).
Capacitation
Sperm capacitation was independently discovered by Austin (1951) and Chang (1951). Capacitation is defined as the process, by which the sperm becomes able to undergo an acrosome reaction in the uterus, then to penetrate and fertilize the oocyte.
The main purpose of sperm capacitation (Fig. 5) consists of hyperactivation in order to reach the oocyte, particularly in the remodeling of sperm membrane with regards to the fusion with the oocyte (Sutovsky, 2011). Capacitation involves a sperm surface remodeling, protein phosphorylation, hyperpolarization, an increased membrane fluidity, internal Ca2+ concentration and pH. A number of different seminal factors have been shown to act as the initial factors of capacitation: fertilization promoting peptide, adenosine, calcitonin, heparin binding proteins and angiotensin II. Other participating messengers are derived from sperm-oocyte interaction. Other factors originate in the female reproductive tract such as leukocytes, progesterone, fertilization promoting peptide, cholesterol, sialic acid binding proteins, capacitation-associated tyrosine-phosphorylated proteins, heparin binding proteins and atrial natriuretic peptide (Storey, 1995; Kumar et al., 2008).
Capacitation requires a period of sperm incubation in the female tract, approximately 1 hour. It involves an increased metabolic activity, higher motility and the removal of the decapacitation factors from the sperm followed by the destabilization of the acrosomal sperm head membrane. This change involves the removal of steroids and seminal glycoproteins from sperm membrane. It allows greater binding between sperm and oocyte. Thanks to Ca2+ permeability, the binding is strengthened. An influx of Ca2+ results in sperm hyperactivation, which induces the higher cAMP level. Ca2+ and HCO3- play a critical role in the regulation of sperm function, most likely by acting as the enzyme effectors involved in signal transduction (Yanagimachi, 1994). Furthermore, the sperm adenylyl cyclase is significantly stimulated by HCO3-. The bicarbonate anion increases an intracellular pH and has been suggested to act as an anion antiport with respect to Ca2+ (Okamura et al., 1985).
The major sperm sterol is cholesterol, among others e.g. desmosterol, desmosterol sulphate, cholesterol sulphate, cholesterol esters, cholestadienol. Additional cholesterol may be obtained from seminal plasma. Cholesterol moves from the sperm membrane to the acceptors and phospholipids into the sperm membrane. The ratio of cholesterol/phospholipids in a freshly ejaculated sperm is about 0.8. Albumin acts as a sink for the removal of cholesterol from the sperm plasma membrane. The loss is initially linear and leads to the exposure of a mannose receptor. Zona pellucida (ZP), an oocyte membrane composed of proteins (70%) and saccharides (30%), contains mannose that interferes with sperm receptors. Cholesterol also inhibits the responsiveness and Ca2+/H+ exchange in the ionophores. It has been suggested that the increased cholesterol level has a role in male unexplained infertility since the concentration is about twice as high as in the fertile subjects. Cholesterol efflux corresponds to an increased level of tyrosine as well as proline protein phosphorylation. The sperm cholesterol level varies among individuals (Mitra and Shivaji, 2005; Jha et al., 2006).
Sperm protein tyrosine phosphorylation (PTP) has been considered to be the key signaling pathway. It is thought that it acts as a signal to alter mitochondrial function. Sperm PTP is dependent on the presence of calcium and bicarbonate ions. It is supported by ATP from glycolysis and is regulated through a protein kinase A (PKA) pathway. However, glucose is thought to inhibit PTP, which could be up-regulated by free radicals, most likely by superoxide anion. Moreover, the superoxide anion generation is also related to sperm lipid peroxidation, hyperactivation and viability (de Lamirande and Gagnon, 1993, Visconti et al., 1998).
Capacitation also involves the membrane hyperpolarization caused by K+ permeability. It has been speculated whether K+ throughput independently allows the recruitment of Ca2+. Subsequently, the membrane potential is increased in tens of mV (Zeng et al., 1995; Visconti et al., 1998).
An essential capacitation factor is a fertilization promoting peptide (FPP), a tripeptide (Glu-Glu-Pro) synthesized in the prostatic glands. FPP is present in SF and comes into contact with sperm after ejaculation. It becomes less active in the female genital tract due to vaginal acidic pH. It has a synergic stimulatory effect with adenosine that increases adenylyl cyclase activity in the sperm. Another seminal protein, semenogelin, appears to block sperm capacitation (Fraser and Osiguwa, 2004).
Sperm proteasome, located on the inner acrosomal membrane, is also involved in capacitation thanks to its proteolytic activity. It assists in protein removal during membrane remodeling, acrosome exocytosis by the degradation of membrane proteins in order to release the acrosomal matrix and to create the so-called acrosomal ghost. The sperm is then prepared to penetrate and fertilize the metaphase II-arrested oocyte (Sutovsky et al., 2004; Zimmerman and Sutovsky, 2009).
Fig. 5 Theoretical trans-membrane and intracellular signaling of sperm capacitation. PKA: protein
kinase A, +/-: stimulating/inhibiting pathways, consequence, reaction, ion exchange. Based on de Lamirande and Gagnon (1993); Zeng et al. (1995); Visconti et al. (1998).
Acrosome reaction
Capacitated sperm becomes hyperactivated with regards to motility. Then, it is able to recognize the oocyte. The sperm membrane is destabilized after capacitation. It can be attached to ZP and undergo an acrosome reaction (AR). Gradual steps are mediated by an osmo-sensitive signal transducing mechanism. An oocyte-sperm fusion is coordinated by the carbohydrate-protein interaction. The carbohydrate-binding site on the sperm interacts with the oligosaccharide ligands of ZP (Topfer-Peterson et al., 2000).
AR (Fig. 6) is defined as the physiological release of acrosomal content. It occurs in the female genital tract following sperm capacitation. It is a precondition to penetrate and fuse the oocyte ZP and to undergo the fertilization event. The cholesterol removal, elevated internal levels of Ca2+ and increased pH during capacitation are thought to trigger the acrosomal exocytosis that reduces the sperm membrane and enables to perceive the oocyte. Acrosomal disruption involves the intracellular/membrane modifications and hydrolytic/proteolytic enzyme release. The most involved enzymes are acrosin and hyaluronidase that are required for oocyte penetration. AR activation and acrosomal exocytosis display the new membrane domains representing the new antigenic targets of the female immune system (Breitbart and Spungin, 1997; Patrat et al., 2000).
AR inducing factors are zona pellucida glycoprotein 3 (ZP3) and progesterone, which is produced by the cumulus cells surrounding the oocyte. It has been shown that ZP binds at least to two sperm plasma membrane receptors, receptor activating phospholipase C (PLC) and tyrosine kinase receptor (TKR), which is coupled to PLC. Binding to a receptor activating PLC influences cAMP elevation and further PKA activation. Binding to TKR leads to the phosphorylation of the calcium transporter that activates phospholipase C (PLC ). Activated
PLC catalyzes the hydrolysis of phosphatidylinositol 4,5-bisphoshate (PIP2) into inositol-triphosphate (IP3) and diacylglycerol (DAG). IP3 binds to a receptor on an outer acrosomal membrane, resulting in Ca2+ release. DAG stimulates phospholipase A (PLA) resulting in fusiogenic lipids (FL) and fatty acids (FA). These substances or their derivates, e.g. arachidonic acid, modulate the AR. The depolarization of plasma membrane by H+/Na+ ionophores increases intracellular pH and activates adenylyl cyclase, which stimulates cAMP elevation and PKA activation. H+/Na+ exchange also alkalizes the cytosol. The increased concentration of Ca2+ and increased pH allow membrane fusion, followed by the AR (Breitbart and Spungin, 1997; Patrat et al., 2000).
Table of contents :
1 INTRODUCTION
2 MALE FACTOR IN REPRODUCTION
2.1 Seminal fluid
2.2 Spermatozoa
2.2.1 Spermatogenesis
2.2.2 Capacitation
2.2.3 Acrosome reaction
2.2.4 Fertilization
3 FEMALE FACTOR IN REPRODUCTION
3.1 Oocyte
3.1.1 Oogenesis
3.2 Embryo development
4 INFERTILITY
4.1 Unexplained infertility
4.2 Immune infertility
4.2.1 Anti-sperm antibodies
4.2.2 Association of seminal components with female sensitization
4.2.3 Auto-immune aspects in infertility
4.3 Mucosal immunity of the female genital tract
4.3.1 Cervical Mucus
4.4 Treatment of female infertility
4.4.1 Fertility drugs
4.4.2 Reproductive assistance
4.4.3 Intravenous immunoglobulins
4.4.3.1 IVIg and infertility related disorders
5 RESULTS
5.1 Publications
5.1.1 Anti-sperm antibodies
5.1.2 Disintegration of human sperm and characterization of its antigen
5.1.3 IgG, IgA and IgE reactivities to sperm antigens in infertile women
5.1.4 Female serum immunoglobulins G, A, E and their immunological reactions to seminal fluid antigens
5.1.5 Immunodominant semen proteins I: New patterns of sperm proteins related to female immune infertility
5.1.6 Immunodominant semen proteins II: Contribution of seminal proteins to female immune infertility
5.1.7 Immunodominant semen proteins III: IgG1 and IgG4 linkage in female immune infertility
5.1.8 Pre-eclampsia: a life-threatening pregnancy syndrome
6 FUTURE ASPECTS
6.1 Design of a miniaturized diagnostic tool
6.2 Immuno-Intervention in female immune infertility
7 DISCUSSION
7.1 Antibody recognition
7.2 Protein markers
7.3 Immunoassay to screen female semen sensitivity
7.4 Immuno-Intervention strategies
8 CONCLUSION
9 PERSPECTIVES
10 REFERENCES
11 LIST OF FIGURES
12 LIST OF TABLES
13 LIST OF ABBREVIATIONS
14 ANNEXES
14.1 Publications not related to the topic of female immune infertility
14.1.1 Tumor markers and their use in clinical practice
14.1.2 Indoor long-term persistence of cypress pollen allergenic potency: a 10-month study
14.1.3 Complementarity between microarray and immunoblot for the comparative evaluation of IgE repertoire of French and Italian cypress pollen allergic patients