Get Complete Project Material File(s) Now! »
Atherosclerosis and decrease in nitric oxide bioavailability
In the cardiovascular system, the deficiency of NO, which is the consequence of either endothelium dysfunction or NO oxidative consumption (increased oxidative or nitrosative stress, decreased antioxidant enzyme activity) is one of the key factors for the initiation and progress of many diseases, including atherosclerosis. As described previously, the endothelium plays an important role in this context, maintaining the balance between vasodilating substances with antiproliferative activity (such as NO) and vasoconstrictor substances with mitogenic properties (such as ET-1) and any disturbance to this balance may cause damage to the arterial wall, by promoting the appearance of endothelial dysfunction. The pathophysiology of endothelial dysfunction is a complex phenomenon, engaging different mechanisms: it leads to vasoconstriction, platelet aggregation, monocyte adhesion and smooth muscle cells proliferation, and has been related to a reduced NO bioavailability, an excess of ROS and an oxidative stress-dependent increase in ET-1 action. NO, one of the most important substance produced by the endothelium, plays a key role in homeostasis maintenance. NO is a gazeous radical with a half-life of ≈ 6– 30 s, continuously synthesized from L-arginine by the nitric oxide synthase (NOS) [118].
There are three distinct isoforms of NOS which differ in structure and function [119]. Endothelial NOS (eNOS) and neuronal NOS (nNOS) are constitutively expressed and are referred as Ca2+-dependent enzymes [120] and generate small amounts of NO for signaling. They are present as dimers, containing a flavin adenine dinucleotide molecule (FAD), a flavin mononucleotide (FMN), a heme group and a tetrahydrobiopterin (BH4), whose absence leads to the production of superoxide rather than NO. These cofactors, together with calmodulin and the NADPH, are needed of enzymatic activity [121]. The third type is the inducible isoform (iNOS), Ca2+-independent and inducible by immunological stimuli [122]. This latter is activated and generates high amounts of NO in response to inflammation [123].
NO is a chemical messenger, particularly in vascular and immune systems playing a critical role in the regulation of a wide range of physiological processes. Its production within the cell is very finely
adjusted to ensure the correct action of NO. Indeed, in physiological conditions, low concentrations of NO (10 nM), which acts as a vasodilator and inhibitor of platelet aggregation, are produced by eNOS, while the activation of iNOS induced during physiopathological processes such as inflammation produces much higher concentrations of NO (> 1 µM). iNOS is expressed physiologically, but is induced by certain inflammatory cytokines (IL-1, INFγ, TNF-α), by LPS and oxidizing agents. This induction is inhibited by glucocorticoids and some cytokines (including TGF-β).
The effect of NO depends on the site of formation, its concentration and the type of targeted tissue. NO released from the endothelium stimulates soluble guanylyl cyclase, producing increased concentrations of cyclic guanosine monophosphate (cGMP). Cyclic GMP interacts with three types of intracellular proteins: cGMPdependent protein kinases (PKGs), cGMP-regulated ion channels, and cGMP-regulated cyclic nucleotide phosphodiesterases (PDEs). Thus, cGMP can alter cell function through mechanism dependent or independent of protein phosphorylation. Depending on the direction of NO release and the site of cGMP activation, differing biological effects can be observed. In vascular SMCs increased cyclic GMP concentrations activate cGMP-dependent kinases that decrease intracellular calcium, producing relaxation [124], whereas increased cGMP in platelets decreases platelet activation and adhesion to the surface of the endothelium [125]. NO can modulate protein activity through three main reactions: Nitrosylation, a reversible coordination of NO to transition metal ions in enzymes, such as ferrous (Fe2+) heme prosthetic groups within the soluble guanylyl cyclase (sGC) enzyme, leading to enzyme activation and increased formation of cGMP.
Protein nitrosation, where NO forms a covalent bond with cysteine (S-nitrosation) or tryptophan (N-nitrosation) residues. Modifications of free cysteine residues present at active sites of effector proteins and peptides subsequently change the activity or function of these proteins. This corresponds to a posttranslational modification of proteins as important as phosphorylation [126, 127]. Numerous studies have focused on the mechanistic aspect of S-nitrosation, however it has also been shown that denitrosation plays a major role in the control of S-nitrosated proteins (Pr-SNO) levels and NO release. S-nitrosothiols can undergo spontaneously or assisted transnitrosation from high molecular weight thiols to low molecular one and inversely.
Nitration, introduction of a NO2 group covalently bound to the aromatic ring of tyrosine or tryptophan residues. These changes are often related to loss of function, due to oxidation or nitration of functionally important residues, as well as the proteolytic degradation of damaged proteins. Nitration mainly consists in the formation of nitrotyrosine, occurring via peroxynitrite in the context of heavy tissular inflammation and oxidative stress. Nitrotyrosine is identified as an indicator or marker of cell damage, inflammation as well as high concentration of NO production and proteins modifications by NO-derived oxidants. Previous studies have demonstrated that nitrotyrosine is enriched in human atherosclerotic lesions and low density lipoprotein (LDL) issued from human atheromas [128].
Endothelial dysfunction would seem to represent the earliest event of the atherosclerotic plaque formation, before a structural lesion of the vessel wall becomes visible [129]. However, the decrease of NO bioavailability can have different other origins, like (i) impairment of endothelial membrane receptors that interact with agonists or physiological stimuli to release NO, (ii) diminished levels or impaired utilization of L-arginine substrate, or BH4 cofactor of the nitric oxide synthase, (iii) reduction in concentration or activity of nitric oxide synthase; (iv) enhanced degradation of NO by oxygen free radicals, (v) impaired diffusion from endothelium to SMCs, (vi) impaired interaction of NO with soluble guanylate cyclase and the subsequent limitation of the increase in intracellular cGMP level, (vii) generalized decrease in smooth muscle cell sensitivity to vasodilators [130]. In turn, diminished NO bioactivity may facilitate vascular inflammation that could lead to oxidation of lipoproteins and foam cell formation, smooth muscle proliferation, extracellular matrix deposition or lysis, accumulation of lipid-rich material, platelet activation, and thrombus formation. All of these consequences of endothelial dysfunction may contribute to the development and clinical expression of atherosclerosis [131].
Finally, several studies have highlighted the relationships between NO, inflammation and oxidative stress, e.g. (i) NO is released during inflammation processes (mainly from induction of the inducible NO-synthase), (ii) NO induces positive or negative effects on vascular homeostasis according to its environment and concentration (with deleterious impact during oxidative stress and inflammation), and (iii) the released NO itself can modulate inflammatory mediators. The reason for such dual effects relates to concentrations, duration of exposure, and production from NO-synthases but also release from the endogenous reservoir represented by S-nitrosothiols (RSNOs), an important storage form of NO. A summary of NO effects related to its concentration and physiopathological conditions are reported in figure 3 (Fig. 3).
S-nitrosothiols: a class of nitric oxide donors
NO, despite being a very reactive molecule, appears to produce effects at distance from its synthesis site. These effects must be mediated by more stable molecules, capable of transporting and storing NO in its active form [132]. Stamler and colleagues postulated the existence of a “NO reserve” in the plasma, in which this radical is in equilibrium with S-nitrosoproteins and/or peptides characterized by a covalent S-NO bond [133]. These adducts have been suggested to play an important role in NO transport, signal transduction pathways and regulation of gene expression [134]. Ignarro and co-workers showed that these adducts could stimulate the conversion of GTP to cGMP in guanylate cyclase and suggested that they are key intermediates in the action of various nitrovasodilating compounds such as sodium nitroprusside and nitroglycerin [135]. In fact, endothelium-derived relaxing factor may be a Pr-SNO adduct.
S-nitrosoalbumin (SNO-Alb) is the most abundant nitrosothiol in human plasma, with concentrations reported to be as high as 5 μM [134, 136]. Many of the high- and low-molecular-weight S-nitrosothiols can release NO either spontaneously or via metabolism, so they are able to mediate many of the biological functions of NO. In addition, Stamler and co-workers [137] proposed that the binding of oxygen to heme irons in Hb promotes also the binding of NO to specific cysteine residues located in the β-subunits of Hb, forming S-nitrosohemoglobin (SNOHb) [137]. Deoxygenation is accompanied by an allosteric transition in SNOHb that releases the NO group. Therefore, SNOHb has been proposed to participate in the regulation of blood flow [137] and platelet aggregability.
The formation of S-nitrosothiols may also play an important role in leukocyte adhesion to the microvascular endothelium. For example, S-nitrosothiols are known to inhibit leukocyte adhesion to microvascular endothelial cells in vivo, presumably via the release of NO. -SH groups are essential for normal leukocyte-endothelial cell adhesion [138]. S-nitrosation of these critical -SH groups on the surface of endothelial cells and/or polymorphonuclear neutrophils (PMNs) could decrease adhesion, thereby limiting leukocyte infiltration. Furthermore, the formation of endogenous antiadhesive S-nitrosothiols by NO- derived nitrosating agents may be inhibited by O2°-, suggesting that during inflammation enhanced O2°-production may promote PMN-endothelial cell adhesion [139]. Indeed it is well established that exogenous NO donors are very effective at inhibiting PMN adhesion in vivo [138, 140]. Formation of S-nitrosothiols may, on the other hand, promote or perpetuate chronic inflammation.
Lander and colleagues [141] have demonstrated that S-nitrosation of one specific cysteine residue on the p21 Ras protein (involved in cellular signal transduction and able to activate genes involved in cell growth, differentiation and survival) in lymphocytes is critical for guanine nucleotide exchange and downstream signaling resulting in the formation of proinflammatory cytokines such as TNF- . Among endogenous RSNOs, the attention was mainly focused on S-nitrosoglutathione (GSNO) and S-nitrosocysteine (CysNO), the most represented low-molecular weight nitrosothiols in vivo. GSNO — formed by the S-nitrosation of reduced glutathione (GSH) — is involved in the storage and transport of NO. It is mostly intracellular inside the vascular wall [142] and may release NO according to the environmental conditions. It exhibits higher stability than NO, mediates protein S-nitrosation processes and is thought to play an important role in vascular signaling and protection, especially in a context of inflammation [143]. The biological activity of GSNO and particularly its vasorelaxant effect have been reported in ex vivo isolated vessel models [144, 145], and is directly linked to its decomposition resulting in the release of NO.
Role of gamma-glutamyl transferase (GGT) in atherosclerosis
γ-Glutamyl transferase is an enzyme widely distributed and conserved in the living world: in bacteria [209], in plants [210] and throughout animal kingdom. In particular, in mammals, GGT is a membrane type II glycoprotein, including a heavy (380 amino acids, 55-62 kDa) and light (189 amino acids, 20-30 kDa) subunits, linked by non-covalent bonds. Through immunohistochemical studies, it has been shown that GGT is located on the membrane of nearly all cells and is preferentially expressed in epithelial tissues with secretory and absorption activity [211]. The highest GGT activity has been found in the kidney, on the luminal surface of the cells of the proximal convoluted tubule, while the cells of the distal tubule and glomeruli are practically free. In the liver, the GGT activity is found in the epithelial cell layer of the extrahepatic biliary tract and liver canaliculi, while, in the pancreas, the most of it is in acinar cells. In the brain the activity of GGT appears to contribute to the functionality of the blood-brain barrier by promoting the metabolism of leukotrienes and detoxification of xenobiotics [212]. GGT is expressed at the endothelial level, by exerting a role in the vascular relaxation, as shown by Dabhould et al, in a rat aorta model, in which GGT activity mediates the release of NO from GSNO [157]. GGT activity is also present on the membrane and intracytoplasmic granules of platelets and granulocytes and lymphocytes, where its increased activity is considered as a marker of differentiation and malignant transformation [213]. The activity of serum GGT is probably due to its release from the cell membranes of various parenchymatous organs, and reflects the quantitative changes in production, release and removal of the circulating enzyme.
GGT is a highly glycosylated glycoprotein and, based on its primary sequence, six possible consensus sequences for N-glycosylation have been identified. N-glycosylation represents 25-30% of the total mass of GGT and it is tissue specific. In fact, purified GGT from different organs has a different molecular weight and, therefore, a different electrophoretic mobility. This heterogeneity of glycosylation suggest the occurrence of « isoforms » for the GGT enzyme, while there are no identified isoenzymes with respect to the amino acid sequence.
Being a cell surface enzyme from the Meister cycle, GGT catalyzes the cleavage of the γ –glutamyl amino acid of L-γ-glutamyl-L-cysteinyl-glycine (GSH) and its conjugates [214]. This is thought to occur through the formation of an intermediate γ-glutamyl enzyme, which then can form free γ –glutamate by hydrolysis, or transfer the γ-glutamyl to other acceptor molecules (e.g. amino acids) through transpeptidation activity.
Macrophages heterogeneity in atherosclerotic plaques
Macrophage functions can broadly be categorized by a series of dichotomies, for example, innate or acquired immunity, tissue destruction or repair, immigration or emigration, cholesterol accumulation or release, pro-inflammatory or anti-inflammatory phenotype. These functions could in principle be carried out by distinct subpopulations of macrophages or, in some cases, lineages related to different monocyte precursors as suggested in the previous chapter.
Actually, M1 and M2 macrophages are thought to represent the extreme polarization phenotypes of a continuum of pro- and anti-inflammatory macrophages all simultaneously present in atherosclerotic lesions. Pro-inflammatory macrophages were found in plaques several decades ago, while M2 macrophages were detected more recently [253]. Stöger et al. [254] studied the distribution of M1 and M2 macrophages in human plaques and showed that both types increase in numbers along plaque progression and are equally distributed in the fibrous cap region. M1-specific cell markers were preferentially detected in rupture-susceptible shoulder regions, whereas M2-specific markers were predominant in more stable plaque regions out of the lipid core in the adventitia [255]. M2-enriched lesion areas expressed high levels of IL-4, a cytokine that is essential for M2 polarization. The observed M2 macrophage population was relatively more resistant to the formation of foam cells and had increased ability to store engulfed cholesterol esters compared to M1 and resting macrophages. M1-specific markers were shown to be increased in carotid atherosclerotic lesions, while M2 markers were preferentially located in femoral atherosclerotic plaques [256]. In addition, plaque M1 macrophages showed up-regulated expression of several MMPs [257]. Indeed, these observations suggest that M1 macrophages are preferentially accumulated in symptomatic and unstable plaques. Therefore, an important aspect is to link the presence of subset-specific surface markers to the actual function of the macrophages in the atherosclerotic plaque. Indeed, the contribution of subsets to the atherogenic process may be better understood, by studying the functions and signaling pathways of the plaque macrophage subsets in more depth, as described in detail in all following paragraphs.
GM-CSF and M-CSF: factors of macrophage differentiation in the plaque
The heterogeneity of macrophages population in atherosclerotic lesions has been a topic of great interest. As previously described, macrophage differentiation means the differentiation of monocytes to macrophages when monocytes infiltrate into the arterial wall and transform from round-shaped cells to irregularly shaped cells capable to intake antigens and migrate within the wall. In humans, blood monocytes are divided in two subpopulations based on CD14 and CD16 expression: CD14+ CD16- are considered as the counterpart of the murine Ly6Chigh monocytes (“inflammatory”) and CD14- CD16+ are the phenotypic equivalent of the murine Ly6Clow monocytes (“resident”) [85, 86, 87] (Fig. 9).
In vitro, monocyte differentiation is driven by two growth factors such as granulocyte-macrophage colony-stimulating factor (GM-CSF) and macrophage colony-stimulating factor (M-CSF) that leads to the formation of macrophages phenotypically similar to M1 (pro-inflammatory) and M2 (anti-inflammatory), respectively [81]. Both, pro and anti-inflammatory macrophages M1 and M2 have been detected in atherosclerotic plaques. M1 cells – widely known as “classically activated” – are characterized by a round morphology. They are involved in the management of Th1-dependent pro-inflammatory immune responses, because they produce a range of inflammatory cytokines – such as IL-1, IL-6, IL-8, IL-12, IL-23 and TNF-α – as well as ROS and NO. On the other hand, M2 cells, known as “alternatively activated”, are characterized by an anti-inflammatory phenotype, with a stretched, spindle-like morphology. They could be induced by Th2 cytokines, and produce IL-10 and various scavenger receptors such as CD36, macrophage scavenger receptor 1, macrophage receptor with collagenous structure and mannose receptor (MRC1 or CD206) [258]. In general, they promote angiogenesis, resolution and repair processes, and tumor progression [259, 90] (Fig. 9).
Mox macrophages associated with atherosclerosis
The additional macrophage phenotype is represented by oxidized phospholipid derived macrophages (Mox) (Fig. 10). In particular, Mox subpopulation has been described to be produced by accumulation of oxidized phospholipids in atherosclerotic lesions.
Mox macrophages show different gene expression patterns and biological functions compared to M1 and M2 phenotypes. Expression of several genes in Mox macrophages is mediated by the redox-sensitive transcription factor Nrf2 [99]. It has been demonstrated that oxidative modification of phospholipids is necessary for activation of Nrf2-dependent gene expression. Nrf2 goes to the nucleus and activates the genes involved in the synthesis of antioxidant enzymes including glutamate-cysteine ligase which is the first enzyme of the cellular GSH biosynthetic pathway [99]. In fact, an increased GSH/GSSG ratio in the Mox macrophages has been described compared to M1 and M2 phenotypes, suggesting that Mox macrophages have the ability to cope better with oxidative stress. Control of redox status in macrophages by Nrf2 may be important in the regulation of several cellular functions that influence tissue homeostasis and inflammation. Hence, an oxidizing environment such as in atherosclerotic lesions, induces the formation of a novel macrophage phenotype (Mox) that is characterized by Nrf-dependent gene expression and may significantly contribute to pathologic processes in atherosclerotic vessels. Defective redox regulation may lead to exacerbated cell death, as seen in chronically inflamed tissue [99].
Differential metabolism in GM-CSF and M-CSF differentiated macrophages
The clear metabolic differences existing between M1 (GM-CSF differentiation factor) and M2 (M-CSF differentiation factor) macrophages contribute to the shaping of their activation state [275]. Arginine catabolism is the most studied metabolism differentiating M1 and M2 macrophages is represented [276, 277]. L-arginine can be a substrate for either NOS which produce L-citrulline and NO, or arginase 1 (Arg-1) which produces polyamines, L-ornithine and urea. M1-derived NO is a major effector molecule in macrophage-mediated cytotoxicity, playing an important role in controlling bacterial and parasitic infections, whilst Arg-1 expression is linked to the wound healing actions of M2 macrophage population [276, 277].
M1 macrophages induce an anaerobic glycolytic pathway, which involves an increase in glucose uptake as well as the conversion of pyruvate to lactate [278]. In parallel, the pentose phosphate pathway (PPP) is also induced following IFN-γ/LPS activation. This pathway generates NADPH for the NADPH oxidase which is important for ROS production. In macrophages, increased lactate formation and activation of the PPP after phagocytosis had been already observed, suggesting potential importance of adapted metabolism on the activation cascade [279]. Additionally, down-regulation of the carbohydrate kinase-like protein (CARKL), which catalyzes the production of sedoheptulose-7-phosphate, is required for the development of a M1 phenotype [280]. Indeed, it has been observed that the drop of NADH levels in cells overexpressing CARKL during macrophage activation, results in a redox shift. PPP activity contributes to the reduction of redox couples via NADPH. Hence, increased GSH and NADH generation are observed during M1 activation while M2 activation resulted in an up-regulation of CARKL, which was not followed by increased GSH or NADH formation. These findings represent a functional distinction between the two polarization states that is CARKL dependent. Hence, CARKL can be considered as a kinase orchestrating pro- and anti-inflammatory immune responses through metabolic control. On the other hand, fatty acid oxidation and oxidative
metabolism are the preferential pathways in IL-4-activated macrophages [281]. IL-4 activates the 67
transcription factor STAT6, which can trigger a pathway inducing mitochondrial respiration [280]. Upon activation, M2 macrophages can drive the pyruvate into the Krebs cycle and can induce expression of components of electron transport chain. Increased glycolysis in M1-polarized macrophages permits to quickly trigger microbicidal activity and cope with a hypoxic tissue microenvironment. In contrast, oxidative glucose metabolism in M2-polarized macrophages provides sustained energy for tissue remodeling and repair (Table 7, see page 75).
Lipid metabolism in GM-SCF and M-CSF differentiated macrophages
Both GM-CSF and M-CSF differentiated macrophages (M1 and M2, respectively) are able to take up lipids in vitro [282, 283] and in vivo [282]. This cholesterol load is accompanied by significant changes in the macrophage transcriptome. Currently, however, it is unclear whether there is a difference in lipid handling between these two types of macrophages. Only few studies focused on this subject and results so far are rather contradictory. Indeed, in primary murine macrophages, genetic profiles of M-CSF differentiated macrophages pointed favorably towards foam cells formation [264]. M-CSF upregulates enzymes involved in cholesterol biosynthesis and downregulates a transporter involved in cholesterol efflux, such as ATP-binding cassette transporter G1 (ABCG1). Moreover, in human monocyte-derived macrophages, oxLDL accumulation was shown to be higher in M-CSF differentiated macrophages than in GM-CSF differentiated cells and correlates with the upregulation of CD36 and SR-A, two membrane proteins involved in the uptake of modified lipids [284]. In particular, oxLDL loading of M-CSF differentiated macrophages causes a shift towards a M1-like phenotype via downregulation of the nuclear transcription Krüppel-like Factor 2 (KLF-2). In agreement with this, uptake of unmodified LDL was also found to be increased in M-CSF compared to GM-CSF differentiated human-derived macrophages [285]. In contrast, GM-CSF differentiated macrophages showed increased expression of several cholesterol efflux regulatory proteins, such as ABCG1, ATP-binding cassette transporter (ABCA1), peroxisome proliferator-activated receptor gamma (PPARγ), liver X receptor alpha (LXRα), all involved in reducing foam cells formation. Moreover, based on CD68 and CD14 expression, Waldo et al. found lipid accumulation in both CD68+/CD14+ (M-CSF-like) and CD68+CD14- (GM-CSF like) cells in advanced human atherosclerotic lesions [282]. In contrast to these studies, Kazawa et al. [283] found an increased uptake and storage of oxLDL in human GM-CSF differentiated macrophages, although they did find ABCA1 and LXRα to be upregulated. Therefore, future studies are necessary to further characterize the difference in lipid handling in these two macrophage subtypes and to determine the contribution of GM-CSF and M-CSF differentiated macrophage in in vivo foam cells formation in atherosclerosis progression. Anyway, macrophages recognize modified lipoproteins through toll-like receptor (TLR2 and TLR4). The scavenger receptor CD36, known to serve as TLR-co- receptor, binds oxLDL and triggers assembly of certain TLR heterodimers, leading to the induction of pro-68 inflammatory mediators implicated in the deleterious effects of oxLDL [286]. The activation of TLR heterodimers, regulated by signals from CD36, leads to the activation of pro-inflammatory signaling pathways involving NFκB, MAP-kinase, ROS-dependent signaling, with an overall switching of macrophage phenotype towards M1. In addition, oxLDL-mediated stimulation of CD36 leads to activation of the inflammasome, which further aggravates vascular inflammation [287, 288] (Table 7, see page 75).
Table of contents :
CHAPTER I
Table 1. Overview of macrophage phenotype observed in human and mice
Table 2. Potential markers of NO bioavailability in human blood
Table 3. Cellular mechanism of GSNO degradation
Table 4. Potential NO donors and their application field
Table 5. Enhancers of NO availability and NO-donating statins and beneficial effects
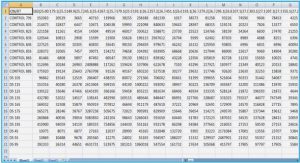
Table 6. Total and fractional GGT activities (mean ± SD, U/L) in both genders
CHAPTER II
Table 7. Characteristics of M1 and M2 macrophages subsets
Table 1. Histological features of the selected plaques used
Supplementary study.
Table 8. GSH and antioxidant enzymes in monocytes, M1 and M2 macrophages
CHAPTER III
Table 1. Distribution of S-nitrosated proteins among distinct cell compartments upon treatment with GSNO
(50 μM) of smooth muscle cells cultured under basal or oxidative stress (50 mM AAPH) conditions.
Table 2. Molecular function and biological implications of cytoskeletal proteins S-nitrosated by 50 μM GSNO
under basal or oxidative stress conditions
CHAPTER I
Fig 2 A. An overview of atherogenesis process: the initial atherosclerotic stage
Fig 2 B. An overview of atherogenesis process: the advanced atherosclerotic plaque
Fig 3. Vascular aspect: NO & physiopathological effects
Fig 4. A model of intravascular metabolism of nitric oxide
Fig 5. The γ-glutamyl cycle
Fig 6. GGT implication in the recovery of extracellular GSH and associated pro-oxidant reactions
Fig 7. Plasma GGT elution profiles: high performance gel filtration chromatography method for GGT fraction
analysis
Fig 8. GGT and cardiovascular mortality
CHAPTER II
Fig 9. Signalling pathways in macrophages involved in atherosclerosis
Fig 10. Polarization process of macrophages in the atherosclerotic lesions
Fig 1. Cytochemical staining for GGT enzyme activity expressed in activated monocytes.
Fig 2. Cytokines in the supernatant of monocyte-derived macrophages
Fig 3. Effects of GM-CSF and M-CSF exposure on cellular GGT expression
Fig 4. GGT release by activated macrophages
Fig 5. Effects of TNFα and IL-10 on GGT expression in monocytes.
Fig 6. Gel filtration chromatography of b-GGT released by TNFα/IL-1-activated monocytes (a) and M1-like
Fig 7. GGT expression in atherosclerotic plaques
Fig 8. Elution profile of GGT activity from whole homogenate of three selected plaque samples (a, b, c)
Supplementary study.
Fig 1. Immunofluorescent detection of specific markers of M1-like and M2-like macrophages
Fig 2. Intracellular nitrite ions production
Fig 3. Quantification of ROS in intracellular and extracellular compartments
Fig 4. Quantification of intracellular GSH.
Fig 5. Evaluation of GSH-dependent enzyme activities
CHAPTER III
Fig 11. Summary of ROS types and sources, and action points of antioxidants
Fig 12. GSH biosynthetic route and GSH cycle
Fig 13. Chemical pathways leading to the formation of protein S-nitros(yl)ation and S-glutathionylation
Fig 14. Mechanisms for oxidant stress-induced modifications on target proteins in cardiovascular diseases
Fig 1. Intracellular and extracellular thiol status in basal and oxidative stress conditions
Fig 2. Extracellular metabolism of S-nitrosoglutathione
Fig 3. Intracellular formation of S-nitrosothiols
Fig 4. Identification and classification of smooth muscle cells proteins S-nitrosated in basal or oxidative stress
conditions
CHAPTER IV
Fig 15. Présentation des perspectives expérimentales concernant le développement d’un modèle de stress
oxydant sur les macrophages
Fig 16. Présentation des perspectives expérimentales sur les cellules musculaires lisses