Get Complete Project Material File(s) Now! »
Infusion of freshly and rapidly isolated VSTs
As traditional ex vivo expanded VSTs require a long generation time (between 10 days to 1 month), patients with acute viral reactions cannot receive VST unless they were prepared for each patient before HSCT, which is cost-intensive and time-consuming and is a brake to the diffusion of this technique. In addition, technically demanding protocols also limit the broad clinical implementation of this method. Although short culture protocols were implemented, it still spends around 10 days to generate VSTs. VST banking should be a good way to rapidly obtain off-the-shelf VST ready for clinical infusion, but the culture process remains time-consuming and cost-intensive mainly to establish a large number of VST lines covering most of HLA types including the rarer [105]. An alternative method has also been developed to freshly isolate VSTs from a leukapheresis by an immunomagnetic strategy using HLA–peptide multimers [76] or IFNγ-capture system [77]. This method is faster (24-48 h), easier and less expensive for broad clinical implementation.
Virus-specific T cells by HLA–peptide multimers
To our knowledge, three investigators[76, 106-108] reported the treatment of post-HSCT CMV infection using adoptive transfer of fresh CMV-specific CD8+ T cells generated by an immunomagnetic strategy based on HLA–peptide multimers from HSCT donors or third-party haploidentical donors. Thirty three patients received CMV-specific CD8+ T cells (dose range from 0.78 to 872×103/kg) for treatment of CMV infections refractory to antiviral drugs. Twenty eight of 32 evaluable patients (87%) achieved complete or partial viral load response (Table 2). Four patients had aGHVD I-III (n=3) or cGVHD (n=1) within one month of CMV-VST infusion. However, three of them had developed previous GVHD before infusion, the remaining one had received a natural killer cell transfusion and an unselected DLI at 21 and 8 days before CMV-VST infusion, respectively.
EBV-VSTs and ADV-VSTs
Uhlin and colleagues only reported one successful experience in the treatment of EBV-associated lymphoma after HSCT [109] and one failure in the treatment of an ADV infection resistant to cidofovir [107] (Table 2). No GVHD associated withVST infusions was observed.
Multimers are most readily made with class I HLA and can only select CD8+ T cells but not CD4+ T-cell subset restricted by class II HLA [110]. In some viral infections, for example ADV infection, immune response is mainly supported by CD4+T cells [77, 111]. Moreover CD4+ T-cells are necessary to support in vivo expansion and survival of CD8+ T cells [75, 112] to maintain virus-specific immune response following adoptive transfer for a long time. In contrast, IFNγ-capture approach can select both CD4+ and CD8+ antigen-specific T cells in an HLA unrestricted manner.
Virus-specific T cells IFNγ-capture system
Recovered peripheral blood mononuclear cells (PBMCs) are stimulated for 6 to 16 hours with a viral antigen [77, 113-116]. These cells are subsequently processed using the Cytokine Capture System (CCS, Miltenyi Biotec) based on an IFN-γ immunomagnetic technology on the CliniMACS device (Miltenyi Biotec), as previously described [117, 118]. This technique can rapidly isolate multi-clone VSTs including CD4+ and CD8+ cells.
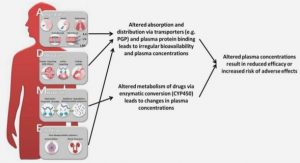
In vitro studies of Immunosuppressive drug effects on T cells or VSTs
Andersson et al tested the effects of FK506 and CsA on cytokine production of peripheral blood mononuclear cell (PBMC) after stimulation with phorbol 12-myristate 13-acetate (PMA) plus calcium ionophore (ionomycin) [131]. They found that both FK506 and CsA significantly inhibited production of IL-2, IL-4, IL-5, IFN- and TNF-. However, the cytokine production was not affected when PBMCs were stimulated with lipopolysaccharide (LPS) and anti-CD28 monoclonal antibody which is a Ca2 +-independent cell activation process [132]. Strauss et al analyzed seven commonly used immunosuppressive drugs (dexamethasone (DEX), mycophenolic acid (MPA), FK506, CsA, rapamycin (RAP), methotrexate (MTX) and cyclophosphamide (CP)) for apoptosis-induction and effector function in human peripheral T cells and cytotoxic T cell lines (CTL) [133]. They reported that antigen specific proliferation of T cells and cytotoxicity of HLA-A1 antigen specific CTL line were only inhibited by CP and MTX among all the tested drugs. CP and MTX also slightly increased activation-induced cell death (AICD) and CD95-sensitivity. Interestingly, they found that DEX, MPA, CsA, FK506 and RAP only prevented activation of naive T cells, but did not block proliferation of activated T cells nor decrease cytotoxic capacity of CTL lines. Zhan et al tested the effect of CsA onto in vitro expanded EBV-VSTs generated by culture [134]. Cytotoxic function of EBV-VSTs against B-lymphoblastoid cell lines (LCL) was moderately inhibited by CsA greater than or equal to 250 ng/mL during a 4 hour assay. However, the cytotoxic function was significantly reduced when EBV-VSTs were cultured with CsA for 7 days before assay, particularly at a dose between 250 and 1,000 ng/mL of CsA. Fuhrmann et al reported that CsA and FK506 were able to reduce IL2 and TNF-α production of CMV-VSTs in post heart and lung transplantation patient, while IFN-γ production seemed less affected [135].
According to in vitro assays, some immunosuppressive drugs, especially CsA, FK506, MTX and Cyclophosphamid were able to decrease T cell proliferation, sometimes targeting mainly naïve T cells, cytokine secretion especially for IL2 and TNF or cytotoxic function of VSTs in case of a long impregnation with CsA. Although an in vitro effect is observed, there is no evidence for a deleterious effect of immunosuppressive drugs on VSTs in vivo. Thus, we report hereafter the VST-clinical studies concerning infusions concomitant to immunosuppressive drug administration.
In vivo studies of Immunosuppressive drug effects on T cells or VST
Doubrovina et al reported Donor Lymphocyte Infusions (DLIs) and/or EBV-VSTs in 49 HSCT recipients with biopsy-proven EBV-lymphoproliferative disease (EBV-VSTs alone: n=17, DLIs alone: n=27, DLIs followed by EBV-VSTs: n=3, and EBV-VSTs followed by DLIs: n=2) [93]. Fourteen patients received immunosuppressive drugs at the time of cell therapy (steroids alone: n=6, steroids combined with CsA or FK506: n=3, sirolimus alone: n=4, CsA alone: n=1). Among the 14 patients who received immunosuppressive drugs, 64% achieved complete response of EBV-disease compare with 74% of the 35 patients who did not receive immunosuppressive drugs. No significant difference was observed. However, by the time cell infusions began, daily doses of systemic steroids had been reduced to 0.07-0.0375 mg/kg of prednisone (median 0.14 mg/kg) or its equivalent. The authors report that analysis of T-cell responses in these patients did not allow ascribing any clear effect of these agents on the expansion of EBV-CTLs in vivo.
Feucht et al treated 30 patients with refractory ADV disease or viremia using ADV-VST infusion [113]. They aimed at a steroid dose of ≤ 1mg/kg prednisolone before ADV-VST treatment. Sixteen patients received steroids at the time of ADV-VST therapy, 12 of 13 (92%) evaluable patients presented in vivo expansion of ADV-VST associated with subsequent virologic response in 12 of 16 (75%) evaluable patients. Moreover, 5 patients still received steroid dose above 1 mg/kg, 3 of the 5 (60%) responded to ADV-VST. The authors stated that in vivo expansion of ADV-VST and virologic response could occur under a low dose of steroids and, in single patients, even under higher doses of steroids. However, only 2 of 7 evaluable patients (29%) who received T-cell–depleting antibodies (antithymocyte globulin (ATG) or alemtuzumab) presented a response to ADV-VST after infusion. The authors considered that treatment with ATG/alemtuzumab seems to decrease the efficacy of ADV-VST. Concerning 2 patients with successful response to ADV-VST despite the use of T-cell–depleting antibodies, they declared that use of ATG/alemtuzumab should not be an absolute contraindication for T-cell therapy. However residual in vivo activity of these antibodies should be detected in future trials.
Mixed Lymphocyte Reaction
Peripheral blood mononuclear cells (PBMCs) from 3 allogeneic blood donors were irradiated (25 Gy) and used as stimulating cells. In vitro expanded ADV-specific T cells were used as responder cells. Stimulating cells (1×105 cells/well) and responder cells (1×105 cells/well) were mixed in a 96-well round-bottom culture plate and incubated for 72 hours at 37°C, 5% CO2. In the same way as proliferative assay, Cell proliferation kit and fluorometer Victor 4® (PerkinElmer, Massachusetts, USA) were used to detect and measure allogeneic proliferation.
Table of contents :
LIST OF PUBLICATIONS AND COMMUNICATIONS
LIST OF ABBREVIATIONS
LIST OF FIGURES*
LIST OF TABLES*
RÉSUMÉ EN FRANÇAIS DU TRAVAIL DE THÈSE
INTRODUCTION
PART I: GVHD AND VIRAL INFECTION INTERACTION
PART II: REVIEW
VIRAL SPECIFIC T CELL TRANSFER FOR THE TREATMENT OF VIRAL INFECTIONS OR DISEASES POST-HSCT
PART III: EFFECT OF IMMUNOSUPPRESSIVE DRUGS IN THE CONTEXT OF GVHD ON VIRUS SPECIFIC T CELLS
OBJECTIVES
RESULTS
ADV-VST SUBPOPULATIONS
Article 1 EFFECT OF IMMUNOSUPPRESSIVE TREATMENT ON ADV-VST
Article 2 SAFETY AND EFFECT OF ADV-VST IN VIVO: A PHASE I/II MULTICENTER CLINICAL TRIAL .
Article 3 DISCUSSION
ADV-VST EFFICACY RELYING ON THEIR COMPOSITION
ADV-VST EFFICACY RELYING ON THE IN VIVO ENVIRONMENT AT THE TIME OF INFUSION.
GVHD AFTER VST INFUSION
PERSPECTIVES
REFERENCES