Get Complete Project Material File(s) Now! »
DWI in ischemic stroke
The time course of signal intensity on DWI and ADC is a dynamic event. Within minutes after ischemia, the decrease of cerebral blood flow causes the disruption of energy metabolism, leading to the failure of the Na+/K+ adenosine triphosphates pump and other ion pumps. This leads to loss of ionic gradients and the translocation of water from extracellular to the intracellular compartment (cytotoxic edema, Figure 10). A restriction of water diffusion in extracellular space occurs, which presents as hypersignal on DW images and hyposignal on ADC map (55). This abnormality can be detected in the first hour following the ischemic stroke while there is still no abnormality on the computed tomography (CT) or other sequences on MRI, such as T2 or FLAIR. (Figure 11) After the initial decrease of ADC, there is a gradual increase of ADC value secondary to the cell lysis and vasogenic edema, with a return to the baseline value known as pseudonormalization around 3-10 days post-onset (56). The signal intensity on DW images is maximal at 40 hours after infarction and then gradually normalizes (57). But the normalization of signal intensity on DW images are delayed compared to ADC value, because DW signal is also influenced by T2 effect. During the chronic stage, there is an increase of water diffusion and also increase in ADC value due to gliosis and cavitation resulted from tissue breakdown.
PWI in ischemic stroke
PWI is an essential sequence in the diagnostic workup of ischemic stroke to evaluate the perfusion status of brain tissue. The parameters mentioned before can be applied to give insights into the hemodynamic status of tissue. (Figure 15) At the hyperacute phase of ischemic stroke, the cerebral perfusion pressure decreases; CBV can be normal or even slightly increased due to an autoregulatory response; CBF remains normal or decreased depending on the success of the compensating autoregulatory vasodilatation; and MTT/TTP/Tmax will be delayed. The infarcted tissue has decreased CBF/CBV and delayed MTT/TTP/Tmax.
Different PWI parameters are used to distinguish the penumbra and the ischemic core. However, no consensus on the parameter thresholds has been achieved. Tmax is currently the most commonly used parameter to define penumbra. It has the advantage of been measured individually with the use of the AIF. Tmax > 2s was used in EPITHET and DEFUSE study to indicate the hypoperfused brain tissue (85,86). Olivot et al. tested 4 predefined Tmax thresholds to calculate the volume of penumbra. They showed that Tmax delay threshold in the range of 4 to 6 seconds provides the best estimation for the hypoperfused brain tissue in acute phase (112). In a comparative study of PWI and PET, Tmax > 5.5 seconds was demonstrated as the best threshold for penumbra flow (< 20 mL/100 g/min on PET CBF) (113). Tmax > 6 seconds was used in several studies to define the critically hypoperfused tissue (36,114). A threshold of MTT delay > 4 seconds beyond the contralateral hemisphere and TTP > 4 and 6 seconds were applied in other studies to define the hypoperfusion (115,116).
T2*-weighted image
To differentiate ischemic and hemorrhagic stroke, CT is considered as reference imaging modality. However, MRI also has high accuracy in hemorrhagic stroke identification. T2*-weighted image is one of the most important sequences to detect intracranial hemorrhage and intraluminal thrombus formation. The detection of acute hemorrhage is based on the paramagnetic effect of deoxyhemoglobin in the red blood cells, which produces inhomogeneity of the magnetic field and causes a susceptibility effect. Therefore there exists a signal loss on T2*-weighted images (48). Besides, intraluminal thrombus can be detected within the occluded vessel in the acute phase of ischemic stroke, providing fast diagnosis of acute thrombotic occlusion. (Figure 19).
Finally, T2* is a sensitive sequence to detect the cerebral microbleeds. The microbleeds appear as round hypointense foci because of the paramagnetic effect of hemosiderin. The presence of microbleed is associated with a spontaneous intracerebral hemorrhage and higher probability of hemorrhagic transformation after thrombolytic therapy (121). An example is demonstrated in Figure 20. However, the criterion of microbleed in excluding stroke patients from thrombolytic therapy remains unclear.
MR angiography
MR angiography is an essential sequence performed in stroke diagnosis workup for vascular evaluation. It can demonstrate the location and extension of the vessel occlusion and therefore provide information in patient selection for reperfusion therapy. 3D-time-of-flight (TOF) is a technique widely used in clinic for intracranial vessel assessment, without the need to administer contrast agent. It is based on the phenomenon of flow-related enhancement of spins entering to an imaging volume, which results in increased signal. It is reliable to identify proximal large-vessel occlusion but less powerful in detecting distal artery occlusion or stenosis. Maximum intensity projection (MIP) is a reconstruction technique usually used to create 3D MR angiography. An example of TOF image and MIP projection is presented in Figure 21.
Procedures of the study
Patients were randomized (1:1) as soon as possible during intravenous thrombolysis to receive intravenous thrombolysis and mechanical thrombectomy (IVTMT group) or intravenous thrombolysis alone (IVT group). Randomization was done with a computer-generated sequence at the coordination center by a computer analyst who was masked to the investigation centers and to the patients.
All patients received intravenous thrombolysis as per standard care — i.e., 0.9 mg/kg of alteplase (maximum 90 mg), with an initial bolus of 10% of the total dose, and then infusion of the remaining dose over 60 min, irrespective of group assignment. For the IVTMT group, if patients had clinically significant improvement, defined as a decrease in the NIHSS score of at least 4 points, angiography and thrombectomy were cancelled. Otherwise, angiography was done and followed by thrombectomy if the modified Thrombolysis in Cerebral Infarction (mTICI) grade was less than 2. The mTICI scale scores perfusion from 0 (no perfusion) to 3 (complete antegrade perfusion of the downstream territory).
For baseline images, MRI or CT were done according to the local routine at each participating center. For MRI, the mandatory sequences were DWI, FLAIR, T2*, and TOF. For CT, an acquisition without contrast and CT angiography evaluating the intracranial vessel were necessary. PWI was highly recommended but not mandatory. Follow-up images were obtained at 24h, discharge/day 7. NIHSS score was assessed at baseline, 24h, discharge/day 7, and 3 months. mRS was evaluated at 3 months.
Main results of THRACE study
402 patients were included in the final analyses of the THRACE study, 202 patients in the IVT group and 200 in the IVTMT group. (Figure 22) The results showed that an approach combining mechanical thrombectomy with standard intravenous thrombolysis provided a significantly higher rate of functional independence at 3 months (defined by a score of 0-2 on mRS) with no evidence of increased mortality than intravenous thrombolysis alone. Bridging therapy seems to be beneficial and should be considered for patients with large-vessel occlusions of the anterior circulation, irrespective of their age, sex, clinical severity, or intracranial location of the occlusion. (31)
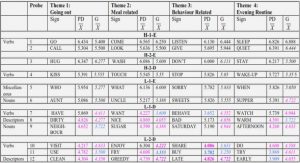
ROI-based parameter value comparison
Intraclass correlation coefficient of ROI-based ADCmean between two readers was 0.98 with 95% confidence interval (CI) 0.96-0.99. Accordingly, the following results are based on measurements obtained by reader 1. ADCmean, rADC, rCBF and rCBV were significantly different between DI and DN: ADCmean was 617.14±54.74×10-6 mm2/s in DI and 677.21±65.67×10-6 mm2/s in DN (p=0.02); rADC was 0.76±0.05 and 0.84±0.08 respectively (p=0.01); rCBF was 0.49±0.15 and 0.63±0.14 respectively (p=0.03); rCBV was 0.80±0.32 and 1.04±0.28 respectively (p=0.04). ADCmean, rADC and rCBF were significantly different in MI and MN: ADCmean was 783.04±37.40×10-6 mm2/s in MI and 821.99±39.73×10-6 mm2/s in MN (p=0.001); rADC was 0.95±0.05 and 0.99±0.04 respectively (p=0.01); rCBF was 0.63±0.18 and 0.71±0.16 respectively (p=0.02). The other parameters showed no significant differences. Results are listed in Table 4.
Patient Selection and Clinical Assessment
We analyzed patients in the THRombectomie des Artères CErebrales (THRACE) trial (Clinical Trial Registration-URL: http://www.clinicaltrials.gov. Unique identifier: NCT01062698), a randomized controlled multicenter trial in France between 2009 and 2015, aiming at comparing intravenous thrombolysis plus mechanical thrombectomy (IVTMT) and intravenous thrombolysis alone (IVT) in patients with acute ischemic stroke due to proximal arterial occlusion, aged 18-80 and with a NIHSS score of 10 to 25. The study design and patient inclusion criteria have been described in detail previously.17 The study protocol was approved by the CPP (Comité de Protection des Personnes) Est III Ethics Committee and the research boards of the participating centers. All patients or their legal representatives provided written informed consent. In this work, we selected patients assigned in the IVTMT group who had an anterior circulation occlusion and qualified pretreatment diffusion-weighted imaging (DWI) data. We excluded patients with severe atrophy or hydrocephaly which could cause inaccurate ischemic location assessment.
Demographic and clinical data and functional outcome were extracted from the THRACE database. Functional outcome at 3 months was measured by modified Rankin Scale (mRS), which consists of 7 grades: from 0 (no symptoms) to 6 (death). mRS was dichotomized into 0-2 versus 3-6, with 0-2 indicating functional independence.
Table of contents :
Chapter 1: Background and state of the art
1.The brain and ischemic stroke
1.1.The anatomy and vasculature of the brain
1.2.Epidemiology of stroke
1.3.Pathophysiology of ischemic stroke
1.4.Treatment of ischemic stroke
1.5.Functional assessment scale for the evaluation of ischemic stroke
1.5.1.National Institutes of Health Stroke Scale (NIHSS)
1.5.2.Modified Rankin Scale (mRS)
2.Utilization of MRI in ischemic stroke evaluation
2.1.Basic concepts of MRI
2.1.1.T1 and T2 relaxation and contrast
2.1.2.Spin echo sequence
2.2.Common MRI sequences used in ischemic stroke
2.2.1.DWI
(1). Principle of DWI
(2). DWI in ischemic stroke
2.2.2.PWI
(1). Principle of PWI
(2). PWI in ischemic stroke
2.2.3.PWI-DWI mismatch
2.2.4.T2-FLAIR sequence
2.2.5.T2*-weighted image
2.2.6.MR angiography
3.Synopsis of THRACE study
3.1.Objective
3.2.Patients inclusion
3.3.Procedures of the study
3.4.Main results of THRACE study
4.Working environment
4.1.Laboratory IADI
4.2.CIC-IT
Chapter 2: The role of MRI in the evaluation of brain tissue viability
Introduction
Article 1
Discussion
Résumé en français
Chapter 3: Pretreatment ischemic stroke lesional volume and clinical outcome
Introduction
Article 2
Article 3
Discussion
Résumé en français
Chapter 4: Ischemic stroke lesional location and functional outcome
Introduction
Article 4
Discussion
Résumé en français
Chapter 5: General discussion
Summary of the results
Strengths
Weaknesses
Implications for the future research
References