Get Complete Project Material File(s) Now! »
Lactic Acid Bacteria
Lactic Acid Bacteria (LAB) represent a group of Gram-positive bacteria which share common characteristics of morphology, metabolism, and physiology. They are acid-tolerant, generally non-sporing, non-respiring cocci or rods, which produce lactic acid as the major end product during the fermentation of carbohydrates. LAB are generally associated with habitats rich in nutrients, such as various food products (milk, meat, vegetables, beverages), but some are members of the normal microbiota of the mouth, the gastrointestinal tract and the vagina of mammals. Based on their major contribution in food and health, LAB are generally regarded as safe (GRAS status).
Lactococcus lactis
Lactococcus lactis, which is defined as the model LAB, is one of the most important microorganisms in the dairy industry and has been identified as a promising candidate for vaccine delivery (LeBlanc et al. 2013). L. lactis cells are non motile cocci, which group in pairs and short chains, and, depending on growth conditions, may be ovoid-shaped with typically 0.5 – 1.5 µm in length. To date, eight sp ecies of Lactococcus have been defined, consisting of L. lactis, L. garvieae, L. plantarum, L. piscium, L. raffinolactis, L. fujiensis, L. chungangensis and L. taiwanensis. Three new species of lactococci have been recently introduced, based on their morphological, physiological and phylogenetic features: L. chungangensis sp. nov., isolated from activated sludge foam (Cho et al. 2008), L. fujiensis sp. nov., isolated from the outer leaves of Chinese cabbages (Cai et al. 2010), and L. taiwanensis sp. nov., isolated from fresh cummingcordia (Chen et al. 2012). Among these species, only L. lactis is found in the dairy industry. Four subspecies of L. lactis can be distinguished: L. lactis subsp. lactis (including the L. lactis subsp. lactis biovar diacetylactis), L. lactis subsp. cremoris, L. lactis subsp. hordniae and the recently proposed subspecies L. lactis subsp. tructae subsp. nov, isolated from the intestinal mucus of trout (Pérezet al. 2011).
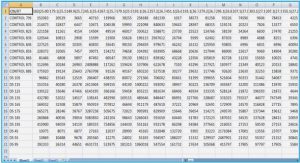
The completely-sequenced genomes of some L. lactis strains (Table I.1) have been published during the last decade, which may provide some important traits in the dairy industry, as well as for other applications. L. lactis strains are of a high biodiversity, exhibiting great adaptation ability for their environment. Indeed, a number of studies have shown that the gene pool plays a pivotal role both in evolution and in the environmental adaptation of L. lactis (Siezen et al. 2005, Górecki et al. 2011, Siezen et al. 2011). A comparative evaluation of the genetic and genomic diversity within a collection of 36 strains isolated from different ecological sources and geographical areas revealed a high variability at both gene and genome levels and gave clues about population structure and evolution. Therefore, the authors proposed a new classification based on ecological separation corresponding to “domesticated” and “environmental” strains (Passeri ni et al. 2010). Similarly, an extensive whole-genome diversity analysis on 39 L. lactis strains, isolated from dairy and plant sources, showed that L. lactis has a very flexible genome: strain variability in terms of functions included proteolysis, lactose fermentation, citrate uptake, metal ion resistance and exopolysaccharides biosynthesis (Siezen et al. 2011).
Application of L. lactis for food and health issues
Application of L. lactis for food products
L. lactis is extensively used in the production of cheese, sour cream and fermented milk (Madigan 2005), which has a significant economic value. As shown in Table I.2, which reports the global sale value of dairy products in 1998, 2003 and 2007, cheese represented about 30% of total dairy products with a 9.8% growth from 2003 to 2007 (Farkye 2004).
Starter cultures consisting of L. lactis are added at the beginning of the cheese making process, which are essential for texture profile and taste of products. L. lactis subsp. lactis is used for making soft cheese while the subspecies cremoris is preferred for hard cheese. Analysis of the L. lactis strains present either in raw milk or from non-dairy source has gained interest in the dairy industry. For instance, for some wild-type lactococci from raw milk, traditional cheese ripening is faster and the flavor is more intense than the one achieved with pasteurized or micro-filtered milk (Corroler et al. 1998). Ayad et al. (Ayad et al. 1999, Ayad et al. 2001) reported the specific-flavor forming abilities of L. lactis isolates from artisanal and non-dairy origin. Wild-type strains produced relatively high levels of primary alcohols and branched aldehydes by degrading amino acids, which could explain their ability to produce distinct flavors. Other examples of L. lactis-based dairy fermented products are kefir and viili. Kefir is a cultured milk beverage from Russia, made with the milk of cow, ewes, goats and buffalos. Kefir is produced by kefir grains consisting of a symbiotic community of 90-95% bacteria (mainly L. lactis subsp. lactis and L. lactis subsp. cremoris) and 5-10% of various lactose-fermenting yeasts (Farnworth 2006). Viili is a type of traditional yogurt from Scandinavian countries and produced by the dual microbial action of LAB and yeasts. The LAB identified in viili include L. lactis subsp. cremoris, L. lactis subsp.lactis biovar diacetylactis (Leporanta 2003).
Moreover, the non-dairy L. lactis strains, isolated for instance from plants, animals and soil, may also offer advantages such as bacteriocin-producing capacities, probably to withstand competition with other bacteria (Ayad et al. 2002). Among 123 strains of LAB isolated from mixed salad and fermented carrots, Uhlman et al. (Uhlman et al. 1992) identified and characterized two Lactococcus strains which produced a heat-stable bacteriocin. This bacteriocin was found to inhibit species of Listeria, Lactobacillus, Lactococcus, Pediococcus, Leuconostoc, Carnobacterium, Bacillus and Staphylococcus. Likewise, the nisin-like bacteriocin produced by L. lactis A164, which was isolated from Korean traditional fermented vegetables, was active against closely related LAB and some food borne pathogens (Choi et al. 2000).
L. lactis as a new potential probiotic
Probiotics are defined as living microorganisms that, when administered in adequate amounts, confer a health benefit on the host (according to WHO – the World Health Organization – and FAO – the Food and Agriculture Organization of the United States). Some criteria have been defined to select a probiotic strain, including its tolerance to the hostile conditions of the stomach and the small intestine, i.e. low pH and bile salts, and its ability to adhere to intestinal surfaces (Morelli 2000). Most of the probiotics belong to LAB and exert their beneficial effects within the gastrointestinal tract (Holzapfel et al. 1998). Possible mechanisms involved are the following: (i) balancing the gut ecology (e.g., reducing harmful microorganisms); (ii) protecting the underlying epithelial cells; (iii) stimulating the body immune response (Vanderpool et al. 2008). Reported beneficial effects of probiotics on host health include the treatment/prevention of some diseases like lactose intolerance (Vasiljevic and Shah 2008), diarrhea, H. pylori infection (Khulusi et al. 1995, Felley et al. 2001, Linsalata et al. 2004), Inflammatory Bowel Disease (IBD) (Gionchetti et al. 2000, Guandalini 2002), mutagenicity and carcinogenicity (Hirayama and Rafter 2000, Lo et al. 2004). The patented probiotic strain L. lactis L1A, which is present in Scandinavian fermented milk, has been shown to have a positive effect on the immune and digestive system. Intake of this probiotic could decrease chronic bowel discomfort following radiotherapy (Henriksson et al. 1995). Another probiotic strain is L. lactis CV56, isolated from vaginal secretions of healthy women and which has been completely sequenced (Gao et al. 2011). CV56 was found to exhibit strong antimicrobial activity by producing nisin A, as well as a greater adhesion ability to vaginal epithelial cells than that of other Lactococcus strains such as L. lactis MG1363. It also contains the genes encoding the riboflavin (vitamin B2) biosynthesis (Capozzi et al. 2012).
Moreover, other studies investigated the potential use of L. lactis as a probiotic. The tolerance to harsh conditions within the gastrointestinal tract was tested for different strains (Kimoto et al. 1999). The strains L. lactis NIAI 527 and L. lactis biovar diacetylactis N7, which are originally from the Japanese National Institute of Animal Industry, exhibited a good ability to tolerate contact with a low-pH juice (pH 2.5), followed by exposure to bile salts at concentrations as high as 0.5 – 0.9% for 30 minutes. A high in vitro adhesion to Caco-2 cells was also observed for the NIAI 527 strain. Furthermore, the strain L. lactis HV219, isolated from human vaginal secretions, was shown to display adaptation properties, i.e. resistance to hostile conditions within the intestinal tract, adhesion capacity to Caco-2 cells and secretion of the bacteriocin HV219 (Todorov et al. 2007). In addition, using a macrophage-like cell line, Kimoto et al. (2004) (Kimoto et al. 2004) demonstrated that the strain L. lactis subsp. lactis G50 was able to induce a high level of cytokines IL-12, IL-6 and TNF-. Accordingly, using the same kind of cell line, Suzuki et al. (2008) investigated the probiotic immunomodulatory activity of 46 different L. lactis strains through their capacity to induce production of the same panel of cytokines (IL-6, IL-12 and TNF-). The extent of induction of IL-6, IL-12 and TNF- was strain-specific and was not related to subspecies, biovariety or the source of the isolates. All these findings converge on the probiotic potential of L. lactis, even though it is undoubtedly strain-specific.
L. lactis as a delivery vector for therapeutic molecules
The use of L. lactis in biomedical applications, as a delivery vector for therapeutic proteins, DNA and vaccine antigens, is a fast-evolving area of interest. During the two past decades, approximately 20 new articles have been published each year (LeBlanc et al. 2013), and have depicted novel strategies, notably for the treatment of human gut diseases (Nouaille et al. 2003). For instance, interleukin IL10-producing L. lactis (Steidler et al. 2003, Braat et al. 2006) and, more recently, Elafin-producing L. lactis (Motta et al. 2012) have provided significant effects against intestinal inflammation. In addition, the use of L. lactis as a delivery vehicle at the mucosal level was reported for DNA (Guimaraes et al. 2006, de Azevedo et al. 2010) or virucide against HIV-1 (Pusch et al. 2005). The example of live lactococci for the treatment of human papilloma virus type 16 (HPV-16) infection was also depicted (Bermudez-Humaran et al. 2005).
As mentioned above, adhesion to intestinal surfaces may be viewed as an important property for the selection of probiotics. The intestinal epithelium is separated from the lumen by the mucus layer. Understanding the structural and functional properties of mucus has gained interest during the past decade. In the next section, we will present the most important findings on this “key” interface within the gastroi ntestinal tract.
Gastrointestinal mucus
Components, organization and functions
Mucus, which lines the gastrointestinal (GI) tract, is directly exposed to a potentially noxious environment and constitutes a protective barrier for the underlying epithelial cells. The mucus layer serves as a selective barrier that prevents from the translocation of toxins, viruses (e.g. herpes simplex virus) (Olmsted et al. 2001, Lai et al. 2010) and pathogens (Johansson et al. 2008), while allowing gases, ions and nutrients to diffuse (Powell 1987, McLaughlin 2002).
Generally, mucus contains water (90 – 98% w/v), muc ins and other components such as salts, lipids, DNA, IgA, defensins. The concentration of mucins, as obtained from the scrapping of pig mucosal surfaces, reaches ~5% (w/v) in stomach/duodenum, ~ 2% (w/v) in small intestine and ~3% (w/v) in colon (Allen 1989). Mucus is also a dynamic layer, which is continuously secreted and transported. Nearly 10 L of mucus are secreted into the GI tract each day with a flow rate of 1-100 µL/s (Cone 2009) . Most of the secreted mucus is then digested and shed in feces. Mucus turnover is balanced by continuous secretion outwards and mechanical erosion that flushes away the external layer containing potentially harmful material (pathogens, drugs, etc.).
Mucins are one of the most important components of mucus. They are extracellular and large glycoproteins. At least 19 human mucin (MUC) genes have been distinguished, cloned and partially sequenced – MUC1, MUC2, MUC3A, MUC3B, MUC 4, MUC5A, MUC5B, MUC6, MUC7, MUC8, MUC12, MUC13, MUC15, MUC16, MUC17 and MUC20, and homologues to many of them have been identified in rodent models (Perez-Vilar and Hill 1999). Mucins can be classified as either secreted or membrane-bound. The secreted mucins confer to mucus its gel-forming properties due to the highly glycosylated regions (see below).
The mucin monomers consist of ~ 80% carbohydrates and the remaining 20% is the protein core, which is arranged into distinct regions. Mucin glycoproteins experience high-frequency domains composed of Pro, Thr and Ser amino acids residues (PTS domains). These domains are often made up by repetitive sequences ordered in tandem and thus referred to as tandem repeats. Flanking the PTS domains are regions that are cysteine-rich (nearly 10%), giving rise to hydrophobic patches (Turner et al. 1999). The PTS domains become highly O-glycosylated within the Golgi apparatus. Once decorated with glycans, the PTS domains form “mucin domains” that have a long and extended rod c onfiguration, like a “bottle brush”. Glycans are composed of 5-15 monomers, including N-acetylgalactosamine (GalNAc), N-acetylglucosamine (GlcNAc), fucose (Fuc), galactose (Gal), and sialic acid or N-acetylneuraminic acid (Neu5Ac) and sulfate residues (Meyer and Silberberg 1979). The mucin O-glycan chain is initiated by a GalNAc attachment to Ser or Thr residues and consists of three regions, named the core, the backbone and the peripheral region.
Pig gastric mucin (PGM) has been widely used for investigating the properties of mucus, such as its rheological behavior (Allen 1989, Celli et al. 2005, Celli et al. 2007). This will be detailed in the section 2.2. In terms of composition, Nordman et al. (Nordman et al. 1997) showed that PGM contains a number of different mucin populations varying in buoyant density, size, “acidity”, glycosylation, sulphation and tissue origin. Furthermore, the analysis of glycan composition showed the prevalence of LacNAc-based O-glycans partially fucosylated in1,2 on Gal residues and sulfated in 1,6 position of GlcNAc residues (Karlsson et al. 1997, Tsubokawa et al. 2007). A schematic representation of PGM is shown in Figure I.1.
Figure I.1. A schematic drawing of the PGM monomer (a); its elementary components (b); PGM dimer (c) and PGM polymer (d) (Bansil and Turner 2006).
The structure and spatial organization of the mucus layer are different according to the intestinal region under study. In the colon, mucus is divided in two distinct physical layers (Figure I.2): (i) an inner layer which is firmly adhering to the epithelial cells and approximately 50-μm thick and (ii) an outer, loose layer which is approximately 100-μm thickness, as measured in rodent models (Johansson et al. 2011). These mucus layers are organized around the highly glycosylated MUC2 mucin, that is secreted by the goblet cells. The inner mucus layer is dense and does not allow bacteria to penetrate, thus keeping the epithelial cell surface devoid of bacteria (Johansson et al. 2008). The inner mucus layer is converted into the outer layer, which is the preferential habitat of the gut commensal bacteria. It can be speculated that bacteria contribute to dissolving the outer loose mucus since germ-free mice exhibit a thicker layer than that of conventional rodents (Johansson et al. 2011). Furthermore, the outer mucus layer has an expanded volume, due to proteolytic activities provided by the host but also probably by commensal bacteria. The numerous O-glycans on the MUC2 mucin not only serve as nutritive substrates for bacteria but also as adhesion sites, thus contributing in this way to the selection of the species-specific microbiota (Juge 2012).
As in the colon, the stomach has relatively well-defined mucus layers made up by the major mucins MUC5AC and MUC6 (McGuckin et al. 2011) (Figure I.2). In the small intestine, in contrast with the stomach and the colon, the mucus layer is rather discontinuous (Figure I.2). Mucus is secreted at the top of the crypts and then moves upward between the villi. Therefore, the tips of the villi are not systematically covered with mucus (Johansson et al. 2011). The main secreted mucin is MUC2, as in the colon.
Figure I.2. Schematic representation of the mucus layer(s) along the gut (Johansson et al. 2011). Note that the thicknesses given are derived from data on rat and adapted from the work of Atuma et al. (Atuma et al. 2001). The symbols in red are representative of the bacteria trapped inside the outer mucus layer. The name of the gel-forming mucins in each intestinal region is indicated. O stands for « outer loose mucus layer » and S for « inner and firmly attached mucus layer ».
Analysis of the O-glycan structures associated with Muc2 in small and large intestines of rats showed that the large intestine was enriched for sulphated residues whereas the small intestine was enriched in sialylated residues (Karlsson et al. 1997). This region-specific glycosylation was also found in humans with a decreasing gradient of fucose from ileum to rectum and an increased gradient of sialic acid (Robbe et al. 2003). This acidic gradient was shown to be acquired after birth, perhaps due to bacterial colonization or initiation of digestive and absorptive functions within the gut (Robbe-Masselot et al. 2009).
Concerning the relationship between mucus and intestinal diseases, numerous studies described the role of alterations in the structure and/or quantity of mucins in initiating and maintaining mucosal inflammation in IBD and in driving cancer development in the intestine, as recently reviewed (Kim and Ho 2010, Sheng et al. 2012). Reduction in MUC2 synthesis and/or goblet cell number, resulting in a barrier defect, was shown to be involved in the onset or development of IBD. For instance, patients with ulcerative colitis (UC) were first characterized by depletion of goblet cells in the colonic epithelium (Theodossi et al. 1994). More recent studies in mouse models of colitis highlighted the importance of mucins in maintaining integrity of the protective mucus barrier, the breakdown of which could result in colitis. Indeed, Muc2-deficient mice, with no morphologically identifiable goblet cells and absence of Muc2 expression in the intestine, were reported to display markedly deficient mucus layers with increased permeability and enhanced bacterial adhesion to the mucosal cell surface. Moreover, these mice developed spontaneous colitis and were more susceptible to dextran sulfate sodium-induced colitis (Van der Sluis et al. 2006). Later, Johansson et al. (Johansson et al. 2013) reported that mucus secreted from human sigmoid colon was normally dense and thick whereas that in patients with active UC was thinner and more penetrable to 2-µm sized fluorescent beads and bact eria.
Table of contents :
INTRODUCTION
Chapter I. Literature review
1. Lactic Acid Bacteria
1.1 Lactococcus lactis
1.2 Application of L. lactis for food and health issues
2. Gastrointestinal mucus
2.1 Components, organization and functions
2.2 Rheological properties of GI mucus
2.3 Mucus microrheology and microstructure
3. Interactions between LAB and mucus
3.1 Determinants of the bacterial cell surface involved in adhesion and muco-adhesion
3.2 Adhesion of L. lactis to the intestinal mucosa and mucus: in vitro and in vivo approaches
4. Identification of the natural L. lactis subsp. lactis isolate TIL448: cell surface determinants and adhesive properties to abiotic and biotic surfaces
4.1. Diversity of L. lactis strains in terms of physico-chemical properties
4.2. Specific adhesion of TIL448 to Caco-2 human intestinal epithelial cells
4.3. Identification and functional role of TIL448 surface proteins in adhesion to Caco-2 cells
Chapter II. Objectives of the study
1. Adhesion and migration of L. lactis TIL448 inside PGM-based hydrogels: role of pili and mucus-binding protein
2. Scrutinizing the microstructure of porcine gastric mucins by fluorescence multiple particle tracking and microrheometry
Chapter III. Results
1. Adhesion and migration of L. lactis TIL448 inside PGM-based hydrogels: role of pili and mucus-binding protein
1.1. Unraveling the Role of Surface Mucus-Binding Protein and Pili in Muco-Adhesion of Lactococcus lactis
1.2. Further investigations on the migration ability of L. lactis inside PGM-based hydrogels
2. Scrutinizing the microstructure of porcine gastric mucins by fluorescence multiple particle tracking and microrheometry
Chapter IV. Discussion – General conclusion
APPENDIX. Experimental protocols for DFT measurements
REFERENCES
LIST OF TABLES
LIST OF FIGURES
SUMMARY IN FRENCH