Get Complete Project Material File(s) Now! »
The role of monocytes and neutrophils (polymorphonuclear cells) in initiation of Clostridium perfringens gas gangrene infections
David K. O’Briena,b, Blair H. Therita, Michael Woodmana, c, Stephen B. Melvillea*
Submitted: August 18, 2006 to Microbes and Infection
- Department of Biological Sciences, 2119 Derring Hall, Virginia Tech, Blacksburg, VA 24061, USA
- Present address: Division of Bacteriology, United States Army Medical Research Institute for Infectious Diseases, Fort Detrick, 1425 Porter Street, Frederick, Maryland 21702, USA
- Present address: Dept. of Microbiology, Immunology, and Molecular Genetics, University of Kentucky College of Medicine, Lexington, KY 40536-0298, USA
- To whom correspondence should be addressed at: Department of Biological Sciences, 2119 Derring Hall, Virginia Tech, Blacksburg, VA 24061, USA, phone: 540-231-1441, fax: 540-231-9307, e-mail: melville@vt.edu
Abstract
Clostridium perfringens is the most common cause of a highly lethal disease, gas gangrene. Established gangrene infections are notable for the rapid spread of the disease and an absence of leukocytes at the site of infection. Yet in the murine animal model, in which bacteria are injected into the hind leg muscles of mice, a large inoculum (1 x 108 – 1 x 109) of bacteria is needed to initiate an infection. This suggests that leukocytes may play a role in inhibiting the initiation of a gangrene infection. To test this hypothesis we used in vitro and in vivo assays to examine the role that monocytic cells and PMNs play in the early stages of a gangrene infection, when bacterial numbers and toxin levels are low. Human PMNs and monocytes effectively killed C. perfringens if complement was present and if the phagocytes and bacteria were actively mixed, allowing for toxin dispersal. In vivo, PMN and tissue macrophages moved into the site of infection when toxin levels were low and the dose was sublethal (1 x 106), but not with a lethal (1 x 109) dose. Also, mice were depleted of PMNs or circulating monocytes before infecting them with increasing inoculums of C. perfringens. In these infections monocytes appeared to play a role in inhibiting a gas gangrene when an intermediate inoculum was used, but PMNs did not enhance survival at any inoculum. Together, these experiments indicate that, in tissues, C. perfringens can be killed by phagocytes when toxin levels are low and that monocytic cells appear to play a more important role in inhibiting a gangrene infection than do PMNs.
Acknowledgements
I would like to acknowledge David K. O’Brien and his work on the mouse studies, performing the PMN depletion study, and the mouse infections. Michael Woodman worked as an undergraduate research student and isolated human PMNs and monocytes and performed in vitro survival assays with Clostridium perfringens. I would like to thank Stephen B. Melville for his guidance in planning and executing experiments and for assistance with results interpretation.
Introduction
Clostridium perfringens is a gram-positive spore-forming bacterium that is the causative agent of gas gangrene. Bacteria are introduced to the tissues through a deep, penetrating wound such as a gunshot or knife wound, crush injury, or intramuscular injection (75). Gas gangrene can occur post-operatively especially following bowel or billiary surgery or improperly performed abortion (75, 129). Spontaneous occurrences of gangrene are most often due to tumors in the gastrointestinal tract (22). It is estimated that there are 1,000 to 3,000 cases of gangrene in the US each year and 80% are due to C. perfringens (75, 100). Fifty percent of patients with the disease develop shock and 40% of these patients die (53). Mortality rates are the highest for cases of spontaneously occurring gangrene, 38%, because of difficulty in diagnosis (100). Post-operative cases of gangrene have a 24% mortality rate and gangrene due to traumatic injury has a 10% fatality rate. Death can occur as quickly as 12 hours if the infection is sudden and severe and if treatment is not immediate (100).
On average, the infection develops within one to three days and ranges between six hours and several days (130, 131). Gangrene is characterized by the sudden onset of severe pain at the site of infection, gas in the tissues, and changes in skin color (131). Inspection of the tissues reveals muscle that does not bleed or contract and connective tissue that is damaged or destroyed. (79, 100). Microscopic examination of the tissue demonstrates rod shaped bacteria, deteriorating tissues, and an absence of inflammatory cells (18, 79, 140). The disease rapidly advances infecting several centimeters of tissue per hour (75). If bacteremia or intravascular hemolysis occurs, the patient will most likely die due to shock (53).
Treatment of gas gangrene must be aggressive and immediate. Infected tissues are removed by debridement or amputation (100, 130, 131) and broad-spectrum antibiotics are administered in high doses for several days. Hyperbaric oxygen has also been shown to be an effective additional therapy and may improve the survival of patients with non-extremity gas gangrene (100, 130).
Gangrene is a highly lethal, rapidly advancing infection in humans. To create this type of infection in mice, a large inoculum is required. The most commonly used mouse model of C. perfringens gas gangrene uses an intramuscular injection of 108 or 109 bacteria (5, 6, 15, 40, 88,140). This infection in mice is lethal, causes severe tissue damage and leukostasis, and the infection advances quickly killing mice within the first 6 to 24 hours of infection. The major virulence factor in gas gangrene, phospholipase C (PLC), has been shown to be necessary for lethality in mice (5, 88). In vivo experiments have also demonstrated that the pore-forming toxin perfringolysin O (PFO), along with PLC, was needed to cause characteristic pathology such as leukostasis and wild-type levels of necrosis in mice (5, 6, 40).
The necessity of a large inoculum to induce a lethal infection in mice may indicate that the immune system is inhibiting the initiation of disease. To test this hypothesis, we examined the ability of polymorphonuclear leukocytes (PMNs) and monocytes to kill C. perfringens in vitro and their ability to move into the site of infection in vivo. We also depleted PMNs and monocytes prior to infection to identify their role in enhancing mouse survival. PMNs and monocytes were able to kill C. perfringens in vitro and to co-localize with C. perfringens in vivo when toxin levels were low. Infection experiments indicated a role for monocytes in inhibiting gas gangrene and enhancing mouse survival when an intermediate inoculum was used, but PMNs did not significantly enhance survival.
Methods
Bacterial strains and growth conditions
perfringens strain 13 (obtained from C. Duncan) was used for all studies. C. perfringens was grown in PGY media (30 g proteose peptone, 20 g of glucose, 10 g of yeast extract, and 1g of sodium thioglycolate per liter) in a Coy anaerobic chamber (Coy Laboratory Products) (162).
Isolation of human peripheral blood neutrophils, monocytes, and serum
Blood obtained from healthy human volunteers was layered on a Histopaque gradient (Sigma-Aldrich). The gradient was centrifuged at 700 x g for 30 minutes at room temperature. The layers containing neutrophils or monocytes were collected and washed twice in Dulbecco’s Modified Eagle’s Medium (DMEM). Sterile distilled water was used for hypotonic lysis of the red blood cells. The viability of the cells was determined to be > 98% using the trypan blue staining. To obtain serum, blood taken from human volunteers was allowed to clot at 37 °C. Serum was collected by centrifugation of the clotted blood at 700 x g for 10 minutes and removal of the supernatant. For heat-treated serum, serum was incubated at 56 °C for 30 min. Human volunteers were recruited for blood donation in accordance with procedures approved by the Institutional Review Board of Virginia Tech.
Bacterial killing assays using human peripheral blood monocytes and neutrophils
perfringens cells were grown to mid-log phase in PGY medium and washed 3 times in phosphate buffered saline (PBS). Neutrophils or monocytes were incubated at a one-to-one ratio in DMEM with washed C. perfringens. For the assays, 1 x 106 neutrophils or monocytes were added to two-ml screw-cap plastic tubes. DMEM and serum were added to bring the volume to 400 µl, as noted, and two µl of bacteria, an inoculum of 1 x 106 bacteria, was added to each tube. Tubes were rotated for two hours at 37 °C. The percent survival was determined by serial dilution in PBS and plating on PGY. For anaerobic assays, the plastic tubes were placed in a Coy anaerobic chamber before the screw-caps were tightened, allowing the oxygen to diffuse out of the tube. When assays were performed using 24-well tissue culture plates, the phagocytes and bacteria were added to each well in the same fashion as stated above for the rotating tube assay.
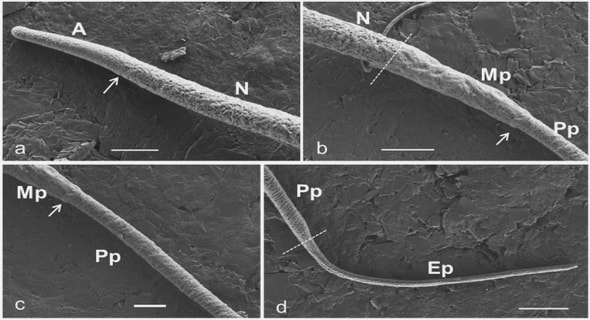
The kinetics of leukocyte recruitment in the early stages of an infection
perfringens was grown to mid-log phase in PGY media and washed twice with PBS. Samples were resuspended in PBS to a final concentration of ~1 x 1010 colony forming units per ml (cfu/ml) or diluted to a final concentration of ~1 x 107 cfu/ml. Twelve BALB/c mice were anesthetized with Isoflurane and inoculated in the right hind leg with 0.1 ml of the 1010 cfu/ml or 107 cfu/ml bacterial suspensions (i.e., 109 or 106 cfu). Three mice were euthanized at ten minutes and one, two, or three hours post-infection. The hind leg muscle was rapidly excised, fixed in neutral-buffered formalin, and stored in 70% ethanol. The muscles were then embedded in paraffin and three µm thick sections were made at two millimeter intervals and the sections were fixed to glass slides. Sections were stained with hematoxylin and eosin and examined for the co-localization of leukocytes (mononuclear and polynuclear) and bacteria. A Leitz Dialux 20 phase-contrast microscope with a Moticam 1300 camera was used to take 30 to 90 random images of bacteria within the tissues for each mouse muscle sample (Table 2-1). The percent of fields with PMNs, monocytic cells, or lymphocytes in the presence of bacteria was enumerated. A field measured 100 µm in diameter at 1000x magnification. The presence of one or more leukocytes co-localizing with one or more bacterial cells within 45 µm was counted as positive.
Preparation of liposomes
Liposomes were prepared as described by Van Rooijen and Sanders (150). Briefly, 33 µg/ml of 1,2 Distearoyl-sn-Glycero-3-[Phospho-rac-(1-glycerol)] (DSPG from Avanti), 33 µg/ml of cholesterol (Sigma), and 100 µg/ml of 1,2 Distearoyl-sn-Glycero-3-Phosphocholine (DSPC from Avanti) were dissolved in 10 ml chloroform. Chloroform was removed by reverse-phase evaporation and the remaining lipid film was dissolved in 10 ml 0.6 M clodronate (Sigma) in water or 10 ml PBS. The resulting solution was evacuated with nitrogen gas and stored at room temperature for two hours. The solution was then put on ice, sonicated for three minutes, and incubated under nitrogen gas at 4 °C overnight.
Before use, the liposomes were washed in PBS three times, resuspended in a final volume of four milliliters of PBS, and kept under nitrogen gas until used.
Depletion of peripheral monocytes
Monocytes were depleted by intravenous tail-vein injection of 100 µl clodronate-filled liposomes (or 100 µl PBS-filled liposomes for control mice). Following monocytic cell phagocytosis and degradation of the liposomes, clodronate is released intracellularly and kills the cell (150). To determine the level of monocyte depletion, 200 µl blood samples were taken from the tail-vein of each mouse before and 24 hours after liposome injection. Each blood sample was stained with F4/80 monoclonal antibody (60) labeled with Alexa Fluor 488 (Molecular Probes) and then treated with Pharm Lyse (Becton Dickenson) to remove red blood cells from the sample. The total leukocyte cell number in each blood sample was determined on a hemacytometer and the number of monocytes labeled with the fluorescently tagged monoclonal antibody specific for the F4/80 surface antigen on monocytes was counted. For each sample the number of monocytes was quantified using fluorescence at 488 nm. Four mice were tested for depletion with each type of liposome.
Depletion of polymorphonuclear leukocytes
Six BALB/c mice received an intraperitoneal (i.p.) injection of 100 µg of the monoclonal antibody RB6-8C5 (Cedarlane), which is specific for the Gr-1 surface antigen present on granulocytes of mice but not on monocytes or lymphocytes (104). RB6-8C5 has been shown to bind and lyse PMNs (113). To verify that PMNs were depleted, blood smears were taken from mice at one, three, and five days post-antibody-injection, and stained using Hema 3 Stain Set (Fisher). The total number of PMNs was enumerated by microscopy (Fig. 2-1). Control mice received similar i.p. injections of PBS instead of the antibody.
C. perfringens infections of depleted mice
Female BALB/c mice were used for all animal experiments. Preceding infection with C. perfringens, mice were depleted of either their PMNs or peripheral monocytes as described above. C. perfringens was grown to mid-log phase and injected into the right hind leg at inoculums of ~1 x 109, 108, 107, or 106 cfu. Once the onset of gangrene was observed, the mice were euthanized to eliminate any unnecessary suffering. Any mouse that did not show signs of gangrene was euthanized 36 hours after the start of the experiment. Six mice were used for each inoculum.
Acknowledgements
Table of Contents
List of Figures
List of Tables
I. General Overview
A. Clostridium perfringens
B. Gas gangrene
C. Phospholipase C
D. Perfringolysin O
E. Listeriolysin O
F. Sialidase
G. Innate Immune System
II. The role of monocytes and neutrophils (polymorphonuclear cells) in initiation of Clostridium perfringens gas gangrene infections
Abstract
Acknowledgements
Introduction
Methods
Results
Discussion
III. Perfringolysin O mutants mediate phagosomal escape of Clostridium perfringens
Abstract
Acknowledgements
Introduction
Methods
Results
Discussion
IV. The characterization of Clostridium perfringens strain 13 sialidases
Abstract
Acknowledgements
Introduction
Methods
Results
Discussion
V. Concluding Remarks
VI. References
Curriculum Vitae
GET THE COMPLETE PROJECT
Investigation of the role of the toxins perfringolysin O (PFO) and sialidase in Clostridium perfringens gas gangrene infections