(Downloads - 0)
For more info about our services contact : help@bestpfe.com
Table of contents
Background
1 Definitions of septic shock
2 Epidemiology of septic shock
2.1 Incidence
2.2 Etiology
2.3 Sites of infection
2.4 Risk factors
2.5 Mortality
3 Immune response in septic shock
3.1 Innate immune system
3.1.1 Activation by microbes
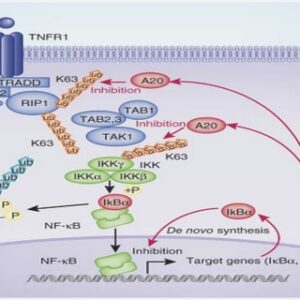
3.1.2 NF-κB pathway
3.2 Adaptive immune system
3.3 Inflammation paradigm
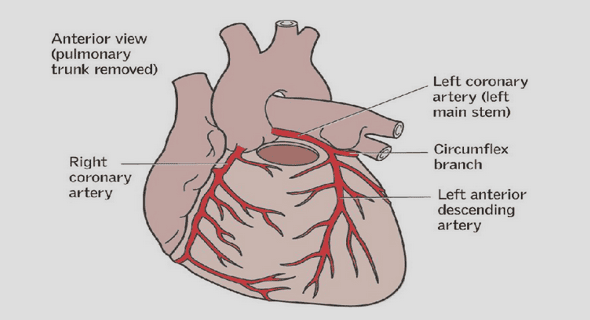
4 Cardiac pathophysiology in septic shock
4.1 Left ventricular dysfunction
4.2 Right ventricular dysfunction
4.3 Mechanisms of cardiac dysfunction
4.3.1 Macrocirculation changes
4.3.2 Microcirculation changes
4.3.3 Autonomic dysregulation
4.3.4 Cytokines
4.3.5 Nitric oxide
4.3.6 Mitochondrial dysfunction
4.3.7 Excitation-contraction coupling impairment
4.3.8 Myofibrillar dysfunction
4.3.9 Cell death
5 Vascular pathophysiology in septic shock
5.1 Vascular regulation
5.2 Vascular hyporeactivity
5.3 Mechanisms of hypovasoreactivity
5.3.1 α1- adrenergic receptor desensitization
5.3.2 Nitric oxide
5.3.3 Prostacyclin and cyclooxygenase -2 pathways
5.3.4 Reactive oxygen species
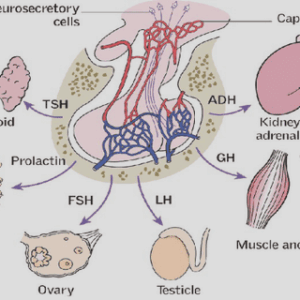
6 Sympathetic nervous system
6.1 β-adrenoreceptors and their signaling pathways
6.2 Sympathetic system in sepsis
6.3 Interaction between sympathetic system and immune system
6.4 How β-adrenoreceptor pathways interact with inflammation
7 Modulation of the sympathetic system at the β1-adrenoreceptor level in septic shock
7.1 Experimental studies
7.2 Clinical studies
8 Pharmacology of used drugs
8.1 Esmolol
8.2 Ivabradine
Objective of the thesis
Methodology
1 Blood pressure measurement by plethysmography
2 Septic shock model
3 Echocardiography
4 Intra-arterial blood pressure measurements
5 Lactatemia assessments
6 Myograph
7 Enzyme-linked immunosorbent assay
8 Protein extractions and concentration measurements
9 Western blots
10 Total RNA extractions and concentration measurement
11 RT-PCR
Study 1
1 Introduction
2 Methods
2.1 Experimental design
2.2 Ivabradine dosage
2.3 Statistic analysis
3 Results
3.1 Model Characterization
3.2 Hemodynamic effects following Ivabradine therapy in septic shock animals
3.3 Vasoreactivity effects following Ivabradine therapy in septic shock animals
3.4 Effect of Ivabradine on circulatory inflammatory mediators
3.5 Effect of Ivabradine on CLP-induced inflammatory pathways in cardiovascular tissues
Study 2
1 Introduction
2 Methods
2.1 Experimental design
2.2 Esmolol dosage
2.3 Statistic analysis
3 Results
3.1 Model characterization
3.2 Hemodynamic effects following different doses of Esmolol in septic shock animals
3.3 Vasoreactivity effects following different doses of Esmolol in septic shock animals
3.4 Effect of different doses of Esmolol on circulatory inflammatory mediators
3.5 Effect of different doses of Esmolol on CLP-induced inflammation in cardiovascular tissues
3.6 Adrenergic modulation following different doses of Esmolol infusion
Discussion
1 Principle results
2 Model characteristics
3 Isolated heart rate reduction by Ivabradine does not improve cardiac or vascular function
4 Isolated heart rate reduction by Ivabradine does not exert any impact on inflammatory patterns
5 Hemodynamic effects of low doses of Esmolol in septic shock animals
6 Immunomodulatory effects of low doses of Esmolol
7 Heart rate reduction or inflammatory modulation of Esmolol
8 Modulation of adrenergic receptor mRNA expression with Esmolol
9 Study limitations
References