Get Complete Project Material File(s) Now! »
CHAPTER 3: LITERATURE STUDY: TOWARDS AN UNDERSTANDING OF TRANSDISCIPLINARITY
“It is no longer enough for health workers to be professional. In the current global climate, health workers also need to be inter-professional” (WHO Report, 2010, p. 36, as cited in Interprofessional Education Collaborative, 2011, p. 13).
INTRODUCTION
This chapter provides a literature study on transdisciplinarity. It commences with an overview of interprofessional care as the backdrop against which transdisciplinarity will be explored. A global and local perspective on interprofessional care is followed by an exposition of transdisciplinarity, consisting of a brief historic overview, various definitions and operational aspects of transdisciplinarity within health and educational care.
INTERPROFESSIONAL COLLABORATION
“Interprofessional collaboration” refers to the use of multiple disciplines in solving a particular problem. In the literature it is also described as interdisciplinary collaboration, integrated care, shared care, joined-up services and wrap-around services, all embedded in ideas of synthesis, union and holism, creating a shared epistemology of confluence (Government, Scotland, 2010; Klein, 1990). Interprofessional collaboration forms part of the evolving field of integrated, holistic service delivery in the face of the increasing need for interdependency in health care and education (Engelbrecht, 2004; Forbes, 2011; Forbes & McArtney, 2010; Klein, 2004; Landsberg, 2011; WHO, 2010). Interprofessional collaboration is a concept of wide appeal to professionals from various disciplines as it seeks to “answer complex questions, explore disciplinary and professional relations and solve problems that are beyond the scope of any one discipline” (Klein, 1990, p. 11). Many models of integrative service delivery, such as pluridisciplinary, multidisciplinary, interdisciplinary and transdisciplinary models, exist under the umbrella term “interprofessional collaboration” (see Figure 3.1). Jantasch (as cited in Klein, 1990), however, describes transdisciplinarity as the ultimate degree of integrative action. He describes interdisciplinarity as a vision infusing all sciences.
I begin this journey towards understanding transdisciplinarity with an introductory discussion of interprofessional collaboration, followed by an in-depth exposition of transdisciplinarity.
Interprofessional collaboration: an international perspective
Although the roots of interprofessional and collaborative practice can be traced back to the beginning of the modern age (Klein, 1990), the WHO’s (1988) release of guidance on the benefits of collaboration among differing disciplines gave international impetus to the development of interprofessional collaboration. It stated the importance of the international trend of teamwork:
Health workers could carry out their numerous tasks more efficiently if they were members of carefully composed teams of people with various types and degrees of skill and knowledge. A team as a whole had an impact greater than the sum of the contributions of its members. (WHO, 1988, p. 7).
Following the above release, the emphasis continued to fall on combining skills to maximise service outcomes. The World Health Report of 2008 (WHO, 2008) advocated person-centred integration among various services and agencies. This health report revealed examples of countries, such as the Democratic Republic of the Congo, where team efforts had proven to bring about positive outcomes in health services. Littlechild and Smith (2013) mention other international drivers of interprofessional collaboration, such as Norway, Iceland, Sweden and Finland, countries where the state plays an essential rol to protect and promote citizen’s socio-economic well being. In these countries, collaborative initiatives, for instance community-based services, have been a continuous development. The authors further postulate a confluence of influences stimulating change:
…the struggle to respond to rising demand for services and the perceived failure of traditional welfare regimes to respond adequately to “users’” needs is due, at least in part, to the failure of the state to work properly “in partnership” with the private and community sectors, and with welfare users (Rummery, 2006, p. 293, as cited in Littlechild & Smith, 2013, p. 27).
Keeping the momentum of promoting interprofessional collaboration as a bolstering strategy against the world-wide workforce crisis in health services, the WHO published the Framework for Action on Interprofessional Education and Collaborative Practice in 2010. This document aims to offer strategies and suggestions to assist health policy makers in implementing “elements of interprofessional education and collaborative practice that will be most beneficial in their own jurisdiction” (WHO, 2010, p. 9). It is therefore clear that interprofessional collaboration is an evolving international principle with widespread implications for service delivery, not only in services of social and health care but also, and specifically of importance for this study, in educational support services.
Interprofessional collaboration in South African health and educational care
Literature on interprofessional collaboration in South African health and educational service delivery is limited. Following the international movement towards integrated and collaborative health care service delivery, a number of South African universities have implemented interprofessional education initiatives for example Mashinggaidze’s (2012) study on the insights and attitudes of students in interprofessional programmes at the Universitu of the Western Cape. Since the country’s entry into a new democratic era, it has distinguised itself from the previous era known for segregation policies. In the former era, interaction among students from different disciplines was not accommodated within health curricula. Students were trained to provide services only within their own discipline (Mashingaidze, 2012). This disjunction among the various health professional programmes resulted in inefficient, isolated service provision that left both service providers and those receiving services frustrated and with a need for holistic, integrated and collaborative service delivery. Equity, community care and a focus on social responsibility play key roles in South African interprofessional initiatives. Pilot studies are launched in communities where resources are scarce. Students from different disciplines, including professions such as occupational therapy, speech and language therapy, physiotherapy and nursing, are placed in rural areas in clinics and schools where they work as interprofessional teams, supervised by the university. Interprofessional education prepares students to act as agents of change towards holistic integrative and collaborative service delivery (Mashingaidze, 2012).
Another example of initiatives to promote interprofessional collaboration and education is a joint project between interprofessional health care student of the Stellenbosch University and the Western Cape College of Nursing. These students are participating in a project where interprofessional education and learning is being implemented Ukwanda Rural Clinic School in Worscester (Theunissin, 2014).
Another initiative undertaken by the University of Stellenbosch to promote interprofessional education and collaboration is the Interprofessional Education and Practice (IPEP) pilot project in Hermanus in the Western Cape. Final year occupational therapy students, medical students and human nutrition studens lived together in a university house and took part in in an interprofessional service-learning early childhood development project (Stellenbosch University, 2013)/
Defining interprofessional collaboration
A broad array of meanings is found in defining the term “interprofessional collaboration”. D’Amour et al. (2005) point out a scarcity of knowledge about interprofessional relationships and its intricacies. This need for knowledge is echoed by a myriad of voices in the literature in their plea for more aggressive research in this nascent field (Léagré, F., Stacey, D., Pouliot, S., Gauvin, F., Desroches, S., Kryworuchko, J., Dunn, S., Elwyn, G., Frosch, D., Gagnon, M., Harrison, M. B., Pluye, P & Graham, I.D, 2011; Thistlethwaite, J, 2012; WHO, 2010).
Klein and Newel (as cited in Klein, 2004, p.1) define interdisciplinary study as “a process of answering a question, solving a problem, or addressing a topic that is too broad or complex to be dealt with adequately by a single discipline or profession”. A literature research project undertaken by D’Amour et al. (2005) revealed the following fundamental aspects in defining collaboration: sharing, partnership, power, interdependency and process. Sharing can refer to sharing of responsibilities, shared decision making, shared principles, shared information, shared planning and shared involvement. The notion of partnership implies more than one partner joining in a collaborative undertaking with a mutual goal in mind. This collaboration among partners is characterised by a constructive, collegial relationship and personal commitment (D’Amour et al., 2005; Friend & Cook, 2007). The nature of this relationship is that of open communication, honesty, trust and respect. Partners are aware of and value each other’s professional contributions and perspectives. Interdependency suggests mutual dependency and synergy, leading to collective holistic action. The fourth concept, power, is created and shared within the relationship. Each partner’s power is recognised by all and is based on his/her contributions rather than title. Partners are valued equally in decision making. Lastly, collaboration is characterised by an evolving process. It is a dynamic and interactive transformative process. The collaborative process can be that of negotiation or compromise in decision making or shared planning and intervention. Friend and Cook (2007) underline this element of process in describing collaboration as a sequential process taking the interaction from beginning to end. D’Amour and Oandasan (in D’Amour et.al., 2011 p. 23) mention the transcendence of professional boundaries in this process: “Communication allows team members to transcend their inclination towards their own field and find common interprofessional territory.”
However, the transcendence of professional boundaries in collaborative health care is not necessarily shared by all. A regulatory body for nurses in Canada, for example, defines collaboration in terms of working together as a team, within the limitations of each member’s scope of practice (World Health Organization, 2008). What all of the above characteristics of interprofessional care have in common is a joining together towards a common goal, defined as “teaming”. A thorough understanding of the concept of teaming is therefore imperative in professional collaboration.
Teaming in interprofessional collaboration
A team can be defined as a number of people joint together in action to fulfil a common goal or purpose for which they accept mutual responsibility (Katzenbach & Smith, 1993).
Within the framework of interprofessional collaboration, partners or members of this team can consist of professionals from various disciplines providing health or support services: “Collaborative practice is an inter professional process … that enables the separate and shared knowledge and skills of care providers to synergistically influence the patient care provided” (Way, Busing & Jones, 2000, p. 3). It can also be a fusion of professionals and patients allowing for the influence of the patient the process of care.
The common goal of all interprofessional collaborative teams is to enhance the quality of care for patients through integration of services and empowerment of patients as active partners in care (Bornman & Uys, 2005a; Bridges et al., 2011; D’Amour et al., 2005; Way et al., 2000; WHO, 2010). To reach this goal, teamwork skills are essential but are often not included in professionals’ training. Developing teamwork skills is an important prerequisite for interprofessional collaboration. Lack of teaming skills is found to be one of the main challenges in the successful implementation of interprofessional collaboration. Core competencies involve cooperation of all professionals in the client-centred provision of care, synchronising one’s own competencies with those of other related professionals and collaborating in decision making and problem solving (Bornman & Uys, 2005a).
The literature presents a number of principles for effective interprofessional teams:
All members provide care to a mutual patient/client.
Common goals for treatment outcomes are developed by the team, and all team members work towards these goals.
Each member is assigned an appropriate role and balance of member participation for tasks. It is important for members to understand each other’s roles.
Members work within a nonpunitive and enabling environment with access to resources.
Clear specifications regarding authority and accountability exist.
Reflection on individual and team performance for improvement takes place. Information is shared through specific procedures.
Mechanisms or processes are in place to oversee execution of plans, assessment of outcomes and, if necessary, adjustment of goals and plans.
Patient and carer empowerment is ensured.
There is consensus among team members regarding ethical principles guiding patient care.
The necessity of research and development is realised.
Professional education and training are provided (Bridges et al., 2011; Interprofessional Education Collaboration, 2011; McConnellogue, 2011; Riley, 1997).
Successful implementation of the above principles relies on clear and open communication, shared problem-solving strategies, skills in conflict resolution and well-defined patient-centred goals. Skills in conflict resolution are of the utmost importance as the diversity of team members’ expertise is a potential source of conflict. Team members must acknowledge conflict in order to process differences in an effective manner (Katzenbach & Smith 1994). Training in communication, conflict resolution and problem solving is found to be part of most interprofessional collaboration education curricula.
Ethics and values in interprofessional collaboration
Interprofessional values and ethics is an emerging aspect of interprofessional collaboration, reflecting a sense of respect and common values. Most recent values and ethical guidelines are provided by the Interprofessional Education Collaborative Expert Panel’s report (2011):
The concerns of patients and the population are at the centre of providing interprofessional health care.
Patient’s privacy and dignity are respected, and information is held in strict confidence by all members when delivering team-based care.
Diversity of cultures and unique differences characterising individuals, population and health care teams are acknowledged and respected.
The unique cultures, beliefs, roles and area of expertise of health professionals are accepted and welcomed.
Professionals cooperate with all stakeholders, including patients, providers of care and individuals or groups contributing to or supporting the health services provided.
Professionals build trustworthy relationships with patients, relatives, communities and other care givers involved.
Ethical dilemmas are managed in line with interprofessional ethical principles based on client-centred service provision.
Professional’s interaction among each other as well as with patients and their families are characterised by honesty and authenticity.
Each professional maintains proficiency in his/her professional discipline appropriate to the scope of practice.
Person-centred approach in interprofessional collaboration
Littlechild and Smit (2013) emphasise the importance of a person-centred approach, reflected in the values of interprofessional collaboration. A person-centred service delivery approach views patients or clients as individuals and places them in the centre of actions rather than fitting them into services. Patients are provided with choices and control in the process, they are involved in setting goals for support and the focus is on highlighting what they may be able to do instead of what they cannot do; in other words, a strength-based approach is followed. The aspect of the patient’s involvement and participation in the support process, however, requires attention as it is important to have a clear indication of what is understood by involvement of and participation by both service providers (professionals) and service users (clients/patients). Roulstone et al. (as cited in Littlechild & Smith, 2013) assert that there is not yet consensus on what participation means in the context of support services. Involvement and participation may vary in degree, depending on professionals’ motivation and commitment to the agenda of patient/client participation (Littlechild & Smith, 2013).
Models of interprofessional care
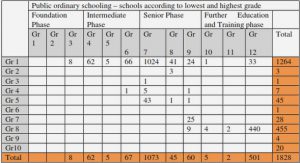
As previously mentioned, a large number of terms exist under the umbrella term “interprofessional”, including “pluridisciplinary”, “cross-disciplinary”, “integrated”, “holistic”, “combined”, “multidisciplinary”, “interdisciplinary” and “transdisciplinary”. Although the main idea across all these terms is the focus on integrated problem solving by collaboration among diverse disciplines, Stock and Burton (2011, p. 1094) warn against the interchangeable usage of these terms, as there are often subtle but significant differences among them: “Terms are either used interchangeably or the term that implies the greatest consideration for what it actually means in terms of the level of integration required.” The three most commonly used models of interprofessional collaboration are multidisciplinary, interdisciplinary and transdisciplinary, each varying in its degree of collaborative practice, as illustrated in Figures 3.4, 3.5 and 3.6. Although the differences are subtle, they are significant in influencing the framing and validity of solving complex problems (Palmen, 2011).
A multidisciplinary service model involves professionals from multiple disciplines addressing a problem. Although the importance of each professional’s involvement is acknowledged, services remain independent. Families will meet with each team member separately, and separate intervention plans are developed according to the relevant discipline. This results in fragmented views of the problem and consequently incoherent therapeutic intervention.
Interdisciplinary collaboration involves a more collaborative approach. Members of different disciplines work together to find a solution to a problem. Regular team meetings are held during which each professional reports according to his/her profession. The team works towards a single service plan and a mutual goal. Fragmentation, however, occurs in the implementation of this plan as members implement parts of the plan according to their various disciplines, resulting in isolated therapeutic intervention. In both of the abovementioned approaches, deficits are treated by therapists in isolation from where the skills are used. Parents and teachers are placed in a recipient, and often subordinate, role as decisions are made by professional team members. They become dependent on the professional’s expert knowledge, failing to empower the people with whom the child spends the most time, leading to a “learned helplessness” that contributes to the already overwhelming need for professional services (Downing & Bailey, 1990).
Although the abovementioned approaches have a collaborative component, they fall short in harmonising with the international trend of integrated holistic service delivery (Downing & Bailey, 1990; WHO, 2010).
The transdisciplinary model has been advocated as the most collaborative in nature. In accordance with this model, a team of professionals from various disciplines shares roles across professional boundaries to maximise integration. A single coherent assessment with all team members present is conducted from which mutual goals and intervention plans emerge. The transdisciplinary model further harmonises with the leading international spirit of collaboration as it is systemic in nature. Communication with and involvement of parents, teachers and other role players in the client’s environment are encouraged and play a critical role. The approach is person-centred, as discussed in section 3.2.6, allowing for parents, teachers and learners to take part in the decision making process. Another attractive dimension of transdisciplinary service delivery is that it fosters an asset-based approach as opposed to the needs assessment found in the medical model. Although needs are identified, the skills and capacities within the client’s social system are accentuated and utilised (Engelbrecht, 2005).
The application of the three described models within the fields of health and education reveals a number of essential differences. Compared to the interdisciplinary and transdisciplinary approaches, a multidisciplinary approach is less integrative in working towards a common goal. Although treatment goals are communicated to other disciplines, each discipline sets its own treatment goals and is solely responsible for reaching these goals. In an interdisciplinary and a transdisciplinary approach, collective goals are decided on and there is a greater level of integration and a higher level of communication among professionals in reaching these goals. What differentiates the transdisciplinary from the interdisciplinary approach is the level of integration when working towards a common goal. In an interdisciplinary approach, professionals stay independent although they are working towards a common goal whereas in a transdisciplinary approach, boundaries among professional disciplines are crossed to maximise integration. Tasks are performed interactively and professional skills and expertise are shared to optimise outcomes (Engelbrecht, 2004). Integration of the system is an important aspect of a transdisciplinary approach. All stakeholders, in the case of learners with BtL the learner, parents, teacher and various professionals, are involved and work towards a common goal (Stock & Burton, 2011).
TRANSDISCIPLINARITY
Transdisciplinarity emerged in the face of a global need to solve complex health and educational problems (Klein, 2004; Saunders, 2011; WHO, 2010). It is a progression from linear interdisciplinary approaches to problem solving whereby existing disciplinary approaches are combined to produce what Colwell and Eisenstein (2001, p. 60) describe as a kaleidoscope for solving complex problems. This metaphor beautifully illustrates the essence of transdisciplinarity:
The word itself is fascinating; it derives from Greek, and roughly means “beautiful form watcher.” When we turn the kaleidoscope tube to create shifting shapes and colors, we watch new and unpredictable patterns and hues appear. At the same time, the elemental components retain their integrity. So it is with the scientific disciplines, which retain their unique viewpoints and insights, but intersect increasingly with other fields to forge new frontiers at every scale.
Muir (as cited in Collwell & Eisenstein, 2001, p. 59) provides us with another useful metaphor for understanding the relevance of transdisciplinarity in solving problems in a complex and interconnected world: “When we try to pick out anything by itself, we find it hitched to everything else in the universe.” Transdisciplinarity strive to describe, explain and find solutions for problems without the restriction of disciplinary boundaries (Palmen, 2011).
History of transdisciplinarity
Prior to the emergence of the systems theory in the mid 20th century, the world was approached through a specialised perspective reflected by the medical model with unidisciplinary service delivery whereby the patient was diagnosed and treated by a single discipline. A practitioner of one discipline acted alone and assumed primary responsibility without actively seeking input from other disciplines and taking into account the multidimensional nature of problems. From this perspective, the world was viewed as an accumulation of fragmented parts to be studied in isolation. The rationale behind this approach was that empirical phenomena could be studied more effectively when specific knowledge rather than broad general information was obtained. The focus was on the different parts, in contrast to the integration of the parts and their complex relation within the whole (Laszlo & Krippner, 1998).
A radical shift away from this perspective happened during the 20th century with the rise of a systemic perspective with Von Bertalanaffy’s (as cited in Drack, Apfalter & Pouvreau (2007) publication of his idea of a general system theory. The concept of “system” suggests a complex of interacting parts together with the relationships among them producing the identification of a boundary-maintaining process. Russell Ackoff (as cited in Laszlo & Krippner, 1998) describes a system as a set of two or more interrelated elements with the following properties: each part has an effect on the functioning of the whole, at least one part of the system affects another part of the same system and these two aspects are present in all possible subgroups of the system. Saunders (2011) remarks that these characteristics of complex systems, arising from the postmodern era, highlight its incompatibility with rational, linear problem solving that applied to the previous dispensation’s reductionistic paradigm of simple cause and effect problems.
By the 1960s systems thinking as a theoretical paradigm began to be known. Parallel to the work of Von Bertalanffy during the 1950s, another theorist, Boulding, unaware of Von Bertalanffy’s work, advocated the integration of social sciences. When Boulding came into contact with Von Bertalanffy’s work, a meeting was held in 1954 between Von Bertalanffy and Boulding; they were joined by two other important role players in the development of knowledge integration: mathematician Anatol Rapoport and physiologist Ralph Gerhard. It was soon evident that their thoughts were remarkably similar although they approached the subject from different directions (Laszlo & Laszlo, 1997). It was during this time that the language of transdisciplinarity came into being. The French psychologist and philosopher, Piaget is known to be the pioneer in using the term “transdisciplinary” at a conference in 1970 where the risk of developing paradigms in social and natural sciences and the potential risks of continuing with discipline specific sciences, in the light of these emerging theories were discussed (Palmen, 2011). Piaget (as cited in Palmen, 2011, p. 2) called for a new perspective of transcending interdisciplinary relations:
Finally, we hope to see succeeding to the stage of interdisciplinary relations a superior stage, which should be “transdisciplinary”, i.e. which will not be limited to recognize the interactions and/or reciprocities between the specialized researches, but which will locate these links inside a total system without stable boundaries between the disciplines.
Many new initiatives have been seen in the decades since 1970. A scientific research centre in France, the Centre for Transdisciplinary Research: Sociology,Anthropology, Semiology, founded in 1973, is the official birthplace of transdisciplinarity. An international initiative was established in 1987 with the International Centre for Transdisciplinary Research and Studies.
Emerging from a research and knowledge production environment, transdisciplinarity soon found its way as an interdisciplinary model of solving complex problems in various fields.
CONTENTS
ABSTRACT
DECLARATION
ACKNOWLEDGEMENTS
LIST OF FIGURES
LIST OF TABLES
LIST OF APPENDICES
ACRONYMS xiv
CHAPTER 1: ORIENTATION TO THE STUDY
1.1 Introduction
1.2 Justification for the Study
1.3 Theoretical Framework
1.4 PROBLEM STATEMENT AND Research Questions
1.5 Research Aims
1.6 Research Method
1.7 Ethics Considerations
1.8 Contribution of the Study
1.9 Definition of Key Terms
1.10 Outline of Chapters
CHAPTER 2: LITERATURE REVIEW: BARRIERS TO LEARNING
2.1 Introduction
2.2 An Ecosystem Perspective on Barriers to Learning
2.3 External Factors Causing Barriers to Learning
2.4 Internal Factors Causing Barriers to Learning
2.5 Identification and Support of Learners Experiencing Barriers to Learning
2.6 Conclusion
CHAPTER 3: LITERATURE STUDY: TOWARDS AN UNDERSTANDING OF TRANSDISCIPLINARITY
3.1 Introduction
3.2 Interprofessional Collaboration
3.3 Transdisciplinarity
3.4 Application of Transdisciplinary Service Delivery in Supporting Learners Experiencing Barriers to Learning
3.5 Benefits of a Transdisciplinary Service Delivery Model
3.6 Challenges of the Transdisciplinary Approach
3.7 Conclusion
CHAPTER 4: CHAPTER 4: EMPIRICAL RESEARCH DESIGN
4.1 Introduction
4.2 Research Aims
4.3 Research Paradigm
4.4 Research Design
4.5 Stage 1: Quantitative Research Method
4.6 Stage 2: Qualitative Research Method
4.7 Data Integration
4.8 Ethics Considerations
4.9 Conclusion
CHAPTER 5: DATA ANALYSIS AND INTERPRETATION
5.1 Introduction
5.2 Analysis and Interpretation of Quantitative Data
5.3 Analysis and Interpretation of Qualitative Data
5.4 Conclusion
CHAPTER 6: DISCUSSION, CONCLUSION AND RECOMMENDATIONS
6.1 Introduction
6.2 Theoretical Framework
6.3 Aim of the Study
6.4 Professionals’ Perceptions of a Transdisciplinary Service Delivery Approach
6.5 Contributions of the Study
6.6 Recommendations
6.8 Conclusion
LIST OF REFERENCES
GET THE COMPLETE PROJECT