Get Complete Project Material File(s) Now! »
The preclinical testing program
The Center for Biologics Evaluation and Research (CBER), the Office of Cellular, Tissue and Gene Therapies (OCTGT) as well as the European Medicines Agency (EMA) have produced guidelines that should to be considered when gene therapy techniques are being developed for clinical application (GTWP, 2008; OCTGT, 2013). The selection of a species/model for investigating gene therapy products must be relevant and best suited to the provision of data comparable to the clinical setting. Immunodeficient animals provide information on the potential for adverse immune responses to the ex vivo genetically modified cells, the vector, or the expressed transgene (GTWP, 2008). Dogs and non-human primates offer good preclinical models for HSC-related protocols with non-human primates being better, due to the fact that they are largely homologous with humans, allowing for nearly all human cytokines to be functional in this model (Watts et al., 2012). Appropriate animal models allow for accurate analysis of the potential toxicity generated by a vector, transgene and cell type, as well as the potential risks of the delivery procedure prior to
clinical trials (Ciurea & Andersson, 2009). The route of administration and the procedures used to administer the product may nullify the therapeutic effect seen in vitro and in animal models. For example, when compared to intravenous delivery, intra-arterial delivery of MSCs avoids the accumulation of the cells in the lungs, allowing the cells more time to migrate to intended tissues (Kean, Lin, Caplan, & Dennis, 2013). The delivery procedure of the manipulated stem cells may require bone marrow conditioning which has an associated morbidity and mortality risk; this risk can however be reduced by carefully selecting an appropriate conditioning regimen (Ciurea & Andersson, 2009). The in vivo behavior and activity of the transduced cells must be determined, including distribution, localization, trafficking and persistence (GTWP, 2008). Scaramuzza et al. (2009) found that CD34+ cells from a WAS patient, intended for gene therapy, proliferated slower in vitro with reduced cytokine receptor production compared with healthy donor cells, thereby affecting the efficacy of the gene therapy (Scaramuzza et al., 2009).
Gene therapy procedures
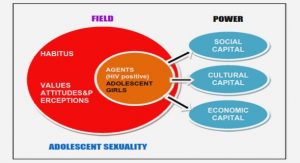
Providing stem cell gene therapies to patients comes with many safety, ethical and socioeconomic concerns, all of which affect the potential success of the therapy (Vattemi & Claudio, 2009). Manipulated stem cells are considered drugs in the USA and in the European Union are classified as Cell-based Medicinal Products (CBMPs) or Advanced Therapeutic Products (Giancola et al. 2012). The handling of these cells has special requirements concerning equipment, safety standard and the training of personnel (Bosse et al. 1997). Appropriate handling conditions include the use of clean room facilities operated according to current good manufacturing practices (cGMP) and require a quality control system (Giancola et al 2012). The production protocols and clinical use of the gene modified cells serve as a basis for the preparation of a risk management plan and the production and distribution of CBMPs. These regulations depend on the relevant national authorities and legislations (Giancola et al. 2012). A cGMP facility is specifically designed as a production facility for the manufacturing of pharmaceutical or cellular products which include the manufacturing space, the raw and finished product storage warehouse and support laboratory areas (Giancola et al. 2012). Furthermore, the vectors used (mostly viral vectors) require an accredited vector production platform that can provide high titer vector samples free of pathogenic contamination and traces of replication competent virus vectors (Bosse et al. 1997; Spencer et al. 2009). The costs involved in establishing these facilities, together with the maintenance and consumable costs, make gene therapy procedures very expensive. This creates uncertainties regarding the financial feasibility of the applications (Mavilio 2012; Soares et al. 2005). From a cost-benefit perspective, the feasibility of such therapies is measured against the costs of current therapies (some of which are life-long) and the life expectancy of patients suffering from the disease to be treated (Jackson and Pepper 2013). Gene therapy can for example be used to potentially “cure” HIV with a once off intervention and thereby allow infected patients to reduce or discontinue highly active antiretroviral treatments (HAART). Although the once off gene therapy treatment is expensive, compared to lifelong HAART treatment it may be more cost effective (Bollinger & Stover, 1999). The economic impact of HIV on countries with high infection rates could be positively impacted (Bollinger and Stover 1999; Jackson and Pepper 2013). The cost of these gene therapies is also anticipated to decrease as the technology develops (Soares et al. 2005; Tremblay 2013).
Chapter 1: Introduction
Aims and objectives
Chapter 2: Clinical safety and applications of stem cell gene therapy
2.1. Introduction
2.2. Safety
2.3. Efficacy
2.4. Gene therapy procedures
2.5. Way forward
2.6. Conclusion
Chapter 3: Clinical applications of genetically modified hematopoietic stem cells
3.1. Introduction
3.2. Clinical trials
3.3 Transgene efficacy and safety
3.4. Source of HSCs used in clinical trials
3.5. Viruses used to transduce human cells
3.6. Virus particle production
3.7. Transduction efficiency
3.8. Engraftment of transduced cells
3.9. Achieving success
3.10. Conclusion
Chapter 4: In vitro analysis of techniques used to expand hematopoietic stem cells
4.1. Introduction
4.2. Materials and methods
4.3. Results
4.4. Discussion
4.5. Conclusion
Chapter 5: In vivo analysis of techniques used to expand hematopoietic stem cells
5.1. Introduction
5.2. Materials and methods
5.3. Results
5.4. Discussion
5.5. Conclusion
Chapter 6: In vitro analysis of techniques used to transduce hematopoietic stem cells
6.1. Introduction
6.2. Materials and methods
6.3. Results
6.4. Discussion
6.5. Conclusion
Chapter 7: In vivo analysis of techniques used to transduce hematopoietic stem cells
7.1. Introduction
7.2. Materials and methods
7.3. Results
7.4. Discussion
7.5. Conclusion
Chapter 8: Opportunities and barriers to establishing a cell therapy programme in South
Africa
8.1. Introduction
8.2. Opportunities
8.3. Weaknesses
8.4. Threats
8.5. Strengths
8.6. Conclusion
Chapter 9: Conclusion