Get Complete Project Material File(s) Now! »
Validation of a semi-automated spinal cord segmentation method
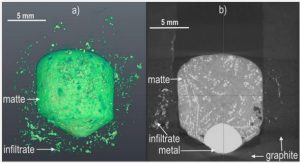
Atrophy quantification from MR images requires as a first step the separation of the spinal cord from surrounding tissues, i.e. CSF, and to delineate white and grey matter if they were visible on the images. Regions-of-interest delineation can be achieved manually or by using semi-automated or automated segmentation methods. Several segmentation methods with varying degrees of manual intervention, reproducibility and accuracy have been proposed to assess spinal cord atrophy from MR images (Horsfield et al., 2010; Zivadinov et al., 2008; McIntosh and Hamarneh, 2006; Tench et al., 2005; Hickman et al. 2004; Coulon et al. 2002; Losseff et al., 1996). Most published studies have used low-resolution T1-weighted 1.5T images and mainly investigated the upper cervical spinal cord in MS patients. However, validation of cord atrophy as a biomarker in spinal cord diseases requires evaluating these segmentation methods in large segments of the spinal cord using high-resolution anatomical MR images generated from actual 3T MRI systems as well as in diseases other than MS. In this respect, MND are characterized by selective neuronal damage that provides relevant models. Indeed, ALS and SMA are characterized by diffuse degeneration of LMN localized in the anterior horn of all spinal cord levels (Katsuno et al., 2010; Wijesekera and Leigh, 2009). The entire CST also degenerates in ALS (Wijesekera and Leigh, 2009). On the other hand, SCI at the chronic phase offers a model of secondary white matter tract lesions due to Wallerian degeneration (Wyndaele and Wyndaele, 2006).
The semi-automated threshold-based segmentation method proposed by Losseff et al. (1996) is one of the most used approaches to quantify atrophy related to its high reproducibility and accuracy.
This method has to be initialized manually by drawing two contours, one to delineate the spinal cord and the other surrounding the CSF. However, this method has only been validated at C2 vertebral level using 1.5T images in MS patients (Horsfield et al., 2010; Losseff et al., 1996).
To validate cord atrophy measurement at 3T using Losseff’s segmentation method, we evaluated its reproducibility, accuracy and robustness to manual initialization at both the cervical and thoracic levels and in neurological disorders other than MS.
Fast and accurate semi-automated segmentation method of spinal cord MR images at 3T applied to the construction of a cervical spinal cord template
In Study 1, we showed that the semi-automated method by Losseff et al. (1996) demonstrated high reproducibility and accuracy for measuring spinal cord cross-sectional area in both cervical and thoracic regions at 3T in normal subjects and in patients with MND and SCI. Improved image spatial resolution obtained at 3T allowed higher segmentation performances than reported previously. More interestingly, full automation of the method seems possible given its low sensitivity to the initialization steps. Losseff’s segmentation method is a semi-automated method, and thus needs a large manual intervention from an operator, which restrains its use to quantify atrophy in few representative slices of the cord region of interest.
In clinical practice, it is often difficult to visually determine spinal cord atrophy. The growing interest in assessing spinal cord atrophy using MRI therefore underlines the need for a fast and accurate segmentation method of the spinal cord with limited manual intervention. This method would also enable segmentation of large data sets in a limited time, thus facilitating investigating in large cord regions using either volume or cross-sectional area measurements. Particularly, this method would enable investigation of the topography of spinal cord atrophy in spinal cord diseases using morphometry methods (Morra et al., 2009; Wang et al., 2010, 2011). Furthermore, to be used, advanced processing methods require an additional step of data normalization. The idea behind data normalization is to adjust for intersubject variability that is not related to the studied pathophysiological process (Mazziotta et al., 2001), as well as to realign all data in the same reference, i.e. template, for statistical comparisons between groups (Vasasina et al., 2012). Several methods have been proposed to construct a template of the cervical spinal cord (Fonov et al., 2014; Valsasina et al., 2012; Stroman et al., 2008). However, the proposed spinal cord templates lacked resolution and accuracy in the construction procedure or used a limited sample of healthy volunteers.
This second study was designed to address two main objectives: i) to construct and validate a new fast and accurate segmentation method with minimal manual intervention benefitting from the high robustness of Losseff’s method to its initialization procedure; ii) as an application, we extended the existing work at 1.5 and 3T (Fonov et al., 2014; Valsasina et al., 2012) to data normalization and the construction of an accurate MRI template of the cervical spinal cord using a large sample of 3T images.
A semi-automated double threshold-based method (DTbM) was proposed enabling both crosssectional and volumetric measures from 3D T2-weighted turbo spin echo MRI scans of the spinal cord at 3T (52 sagittal slices, FOV=280 mm, voxel size=0.9×0.9×0.9 mm3, acquisition time ~6 min). Eightytwo healthy subjects, 10 patients with ALS, 10 with adult SMN1 gene-linked SMA and 10 with SCI were studied. The DTbM was compared with active surface method (ASM) (Horsfield et al., 2010) and Losseff’s segmentation method (Losseff et al., 1996), two of the most used segmentation methods to quantify atrophy (De leener et al., 2016a), taking manual outlining from an experienced operator (with four years’ experience) as the ground truth. An independent expert neuroradiologist (with seven years’ experience) visually scored DTbM and ASM segmentations in cervical and thoracic cord regions. The operator was blinded to the type of data and methods. Accuracy was also quantified at the cervical and thoracic levels as well as at the C2 vertebral level. Fifty-nine MR images from healthy subjects were used to construct a cervical spinal cord template and a standardization pipeline was designed.
In this second methodological study we designed a segmentation method with minimal manual intervention as well as a data normalization pipeline. Visual scoring showed better performance for DTbM than for ASM in both healthy and pathological groups (Table 3). More importantly, the neuroradiologist did not find any visual abnormalities in most cases of ALS and SMA data, justifying the need for quantitative methods to analyze MND data, which represented one of my main scientific focus during my thesis. Quantitative accuracy analysis showed that DTbM outperformed ASM at both cervical and thoracic spinal cord levels as well as at C2 vertebral level in both healthy and pathological groups, confirming the visual evaluation results (Tables 4 and 5). Our method showed similar accuracy compared with Losseff’s method, but with the advantage of limited manual interaction. An accurate data normalization pipeline was designed that included DTbM, enabling the construction of an accurate straight cervical spinal cord template and a tissue probability map (Figure 3). Our segmentation method may also accurately measure cross-sectional area and spinal cord volume in a large range of pathologies. More interestingly, the proposed tools could be used to investigate the topography of spinal cord atrophy in spinal cord diseases using morphometry methods (Morra et al., 2009; Valsasina et al., 2012, 2013; Rocca et al., 2013). Among these methods, surface-based morphometry was used to map cord atrophy in the context of adult SMN1-linked SMA (Study 5).
Electrophysiological and spinal imaging evidence for sensory dysfunction in amyotrophic lateral sclerosis
Animal and human studies in ALS showed evidence of involvement of spinal and cortical interneurones, and structures such as corpus callosum, basal ganglia and the cerebellum (Prell and
Grosskreutz, 2013; Thivart et al. 2010; Pradat et al., 2009; van der Graaff et al. 2011; Carr et al. 2010; Özdinler et al., 2011; Shefner and Logigian, 1998). In addition, post-mortem examinations of spinal cords in ALS patients have shown axonal loss within the dorsal roots suggesting an alteration of the sensory afferent pathways at late stages of the disease (Kawamura et al., 1981; Averback and Crocker, 1983; Bradley et al., 1983). Peripheral and central degeneration of sensory pathways have also been reported in presymptomatic ALS mice, suggesting that the sensory defect occurs at a very early stage of the degenerative process (Sábado et al., 2014; King et al., 2012; Guo et al., 2009). Electrophysiological studies showed evidence of sensory abnormalities that increase with disease severity in ALS patients (Constantinovici, 1993; Gregory et al., 1993; Cosi et al., 1984). Therefore, the question of whether these alterations are consecutive to motoneurons loss, or could act as a primary debilitating mechanism of the disease remains an open question.
In a previous study of ALS patients (Cohen-Adad et al., 2013), by using DTI and MT imaging, we showed that the dorsal column, i.e. pathways conveying peripheral sensory information to supraspinal structures, were altered. Diffusion tensor imaging also revealed dorsal column abnormalities in a subset of 12 patients with early onset (median/maximum disease duration 9/12.6 months). This latter, and unexpected, result suggests that the sensory afferent pathways to spinal and cortical structures might already be affected at an early stage in ALS, and thus that the sensory alteration may indeed participate in ALS pathogenesis. However, MRI does not allow a functional exploration of the pathways, spinal and/or cortical, fed by sensory afferents. Therefore, it is now necessary to verify if the anatomical changes observed with MRI in ALS patients are correlated to a dysfunction of sensory feedback integration.
The objective of the present study was to investigate the anatomo-functional properties of sensory
pathways in ALS patients with distal motor dysfunctions in upper limbs and no sensory symptoms,
combining spinal DTI and SEP.
Multi-parametric spinal cord MRI as potential progression marker in amyotrophic lateral sclerosis
Recent works by our team and others showed that multi-parametric MRI approaches (DTI, MT and atrophy measurement) allow quantification of lesions in ALS (Cohen-Adad et al., 2013; Agosta et al., 2009; Valsasina et al., 2007) and detection of infraclinical lesions (Study 3). In addition, we showed that some metrics correlated with LMN involvement, which is reflected by cord atrophy, as assessed by transcranial magnetic stimulation (TMS) results (Cohen Adad et al., 2013). Importantly, we showed a correlation between cord atrophy in ALS patients and clinical disability (Cohen-Adad et al., 2013), that was later confirmed in an independent cohort (Branco et al., 2014). In the context of ALS, which among the neurodegenerative diseases is characterized by its fast progression, investigating the progression of lesions is a major challenge. From a pathophysiological perspective, there is a growing interest in the mechanisms of propagation of ALS with the emerging hypothesis of prion-like propagation (Pradat et al., 2015). Neuroimaging methods appear as necessary tools to study in-vivo the temporal and spatial pattern of propagation (Pradat et al., 2015). Longitudinal studies are also mandatory to test and validate biomarkers of progression that are an unmet need for monitoring disease progression at the individual level and to provide surrogate markers of efficacy in clinical trials (Annex A). The development of high motor disability and respiratory insufficiency with orthopnea are classical limitations for performing longitudinal studies in ALS patients.
The main objective of the present study was to test the hypothesis that spinal cord MRI was able to detect in-vivo the progression of the neurodegenerative lesions in ALS. The second objective was to test whether the changes of MRI metrics were clinically meaningful, that is, a major criteria for biomarker development, by investing correlations with functional decline.
Table of contents :
Contents
Remerciements
List of Tables
List of Figures
Glossary
Abstract
Publications
Articles arising from this work
Additional contributions
1. Introduction
2. Background
Motor neuron diseases
Historical setting
Amyotrophic lateral sclerosis
Spinal muscular atrophy
Spinal cord MRI
Principals of MRI
Challenges
Clinical setting
Research setting
Advanced MRI
3. Objectives
4. Results
Methodological studies
Study 1 – Validation of a semi-automated spinal cord segmentation method
Study 2 – Fast and accurate semi-automated segmentation method of spinal cord MR
images at 3T applied to the construction of a cervical spinal cord template .
Multi-parametric MRI studies in MND
Study 3 – Electrophysiological and spinal imaging evidence for sensory dysfunction in amyotrophic lateral sclerosis
Study 4 – Multi-parametric spinal cord MRI as potential progression marker in amyotrophic lateral sclerosis
Study 5 – Cervical spinal cord atrophy profile in adult SMN1-linked SMA
5. Discussion
Methodological developments
Multi-parametric MRI studies in MND
Perspectives
Annex A
Annex B
References