Get Complete Project Material File(s) Now! »
Polymeric carriers for NO
A polymeric carrier is interesting for the delivery of NO to its specific site of action. Because of the short half-life of NO and the side effects of several NO-donors, there is a need to develop polymeric delivery systems which could deliver NO to the site of action for a long period of time and avoiding harsh GIT conditions by inclusion in polymers.
In this thesis, we used thiolated polymers also known as thiomers because they have been investigated for therapeutic purposes. Since, thiolated polymers have a free thiol group, NO could be linked and can be delivered for its specific site of action. Thiomers are meant to be used for mucoadhesion purposes because the free thiol group of thiomers can link with the glycoprotein of the mucous in GIT. This occurs via disulfide bonds but we can also utilize this free thiol group to link NO and can be the final compound to be used as a NO carrier. We also used non-biodegradable polymers (Eudragit® FS 30D) for direct encapsulation of NO-donor (GSNO) for specific intestinal delivery.
Micro/nanoparticles
Pharmaceutical companies widely used drug delivery technologies to expand market for already established products. It has been realized in the past two decades that nanotechnology is a fundamental part of drug development, which results in designing a wide range of drug delivery systems. It also progressively increase the number of commercially available nanotechnology based drugs which can reduce side effects, facilitate drug administration, improve patient compliance, decrease drug toxicity, enhance bioavailability of drugs and can be used as site specific therapeutic targeted delivery systems (Saraiva et al., 2011). Nanoparticle drug delivery systems has become a widely studies strategy for increasing solubility and tissue specificity (Polizzi et al., 2007). Furthermore, incorporation of drug in nanoparticulate system can reduce renal and hepatic clearance thus optimizing the drug’s pharmacokinetics properties and biodistribution (Orive et al., 2005). In biomedical applications, the encapsulation of drug in nanostructures is a significant subject because it can increase the drug stability and solubility. Furthermore, it prolongs the drug release rates and decrease toxicity. A variety of nanostructures are used for these purposes including polymeric nanoparticles, solid-lipid nanoparticles and liposomes etc.; that’s why, polymeric nanoparticles appears as an interesting carrier for NO-donors (D Marcato et al., 2013b). Hence, nano-carriers may facilitate the development of multifunctional systems for targeted drug delivery of therapeutic outcome (Bae et al., 2005).
Recent studies showed extensive investigations on the use of polymeric nanoparticles. It is suggested that polymeric particulate systems can modulate drug activity by passive or active targeting to different tissues. Biodegradable polymers can degrade into non-toxic monomers inside the body, which are usually highly stable in biological fluids as well as during preparation and storage (Kanayama et al., 2010; Saraiva et al., 2011). Some reports have been published on the polymeric delivery of NO (Marquele-Oliveira et al., 2010). The therapeutic and effects of NO prodrugs can be enhanced by incorporation into nanoparticles composed of polystyrene-b-PEG (Jain et al., 1998). In another study, NO was efficiently delivered to the vaginal mucosa by using PLGA, which results in improved blood perfusion and having an implication on female sexual dysfunction (Yoo et al., 2010).
Non-biodegradable polymers : Eudragit®
The polymers that are stable in biological system are known as non-biodegradable polymers. These are used as drug carriers and include polymethylmethacrylate, polysilicones and ethylene-vinyl acetate copolymers (Galaev and Mattiasson, 2007).
Eudragit® is the brand name for a variety of copolymers based on polymethacrylates marketed by Evonik Industries, Germany. It was first introduced by Rohm & Hass GmbH, Darmstadt in 1953 as an alkaline soluble material for drug coating purposes resistant to strong stomach acids. Later on, this brand diversified gradually to anionic, cationic as well as neutral copolymers based on methacrylic acid and methacrylic or acrylic esters or their derivatives in varying ratios. These polymers exhibited varying degree of pH dependant and/or independent solubility’s. Eudragit® polymers are extensively used for pharmaceutical coatings, matrix formers in common granulation techniques and in direct compression (Thakral et al., 2013). Different types of Eudragit® are commercially available and could be obtained as dry powder, an aqueous dispersion or as an organic solution (Kola and Kumar). These copolymers acts as polyelectrolytes and are suitable for soluble gastro-intestinal drugs delivery as well insoluble but swellable delivery systems (Animesh et al., 2012).
Intestinal barriers to the absorption
The alimentary canal from mouth to anus is covered with a mucous membrane called as mucosa, which serves as a first barrier for materials to enter into the body. The mucosa is composed of a thin epithelial layer having loose connective tissues (lamina propria) that contains blood and lymphatic capillaries. Absorption of a substance from lumen of the elementary canal occurs when the substance passes through the epithelium, a part of lamina propria and the walls of blood and lymph capillaries. Substances can also pass through the junctions between epithelial cells. Moreover, the absorption of orally ingested materials takes place mainly in the small and large intestines (DeSesso and Jacobson, 2001). However, to form an intact epithelial barrier, the paracellular space should also be sealed. This paracellular seal is provided by the tight junction. Tight junctions cannot be seen well by light microscopes but they can be localized on hematoxylin and eosin-stained slides. However, transmission electron microscopy shows the tight junctions to be discrete rejoin of membrane apposition between adjacent epithelial cells at the luminal aspect of the apical junction aspect. The adjacent plasma membrane appears to fuse at this site which leads to the initial misinterpretation of the light junction as impermeable membrane (Clayburgh et al., 2004).
Immunosuppressive drugs
Patients with moderate to severe activity of CD are treated with traditional drugs like corticosteroids, which is the main therapy for such type of diseases. Corticosteroids induce the remission of symptoms in a high percentage of patients. Due to the different side effects produced by systemic steroids like Cushing syndrome, osteoporosis, diabetes and infection (Lichtenstein et al., 2006), a glucocorticoid derivative known as budesonide has been introduced few years ago. It is supplied as sustained-release microgranules and it acts on local mucosa and has positive results. Intravenous immunoglobulin (IVIG) has also been used in the management of aminosalicylate and steroid resistant CD for more than 20 years (Rogosnitzky et al., 2012). The use of immunomodulators is complicated because of delayed onset of action and having serious side effects like bone marrow suppression, hepatotoxicity and pancreatitis. The use of both immunomodulators and corticosteroids also have a high effect on immune system and can increase the risk of serious and fatal infections in patients been treated with these drugs (Lichtenstein et al., 2006).
An immunosuppressive drug, methotrexate, is also used to treat CD. It is having side effects more common when used in high doses; however, no serious side effects have been observed. Some of the common side effects include nausea, vomiting, abdominal pain, diarrhea, skin rash and headache (McDonald et al., 2014).
Anti-tumor necrosis factor therapy (TNF-α, tumor necrosis factor α) is an important therapy used in the treatment of patients with CD (Colombel et al., 2004). The chimeric anti-TNF-α, infliximab, is also an effective drug in closing fistulas in CD’s patients (Lichtenstein et al., 2005). TNF-α is a pro-inflammatory cytokine, which is elevated in the stool, mucosa and blood of patients with CD (Hanauer et al., 2006), is having an important role in the pathogenesis of CD. Infliximab binds to TNF-α and neutralizes its biological activities; when given as a 5 mg/kg (IV infusion), infliximab induces remission in patients with moderate to severe CD (Rutgeerts et al., 2004). It reduces corticosteroids requirements (Rutgeerts et al., 2004) and facilitates closure of symptomatic fistulas in CD patient’s, which results from inflammation penetrating from effected bowel into adjacent organs, tissues or skin. It is estimated that about 20 – 40% of individuals with CD will develop it over the life-time of the disease. Fistulas closure was observed in patients when a 3-dose regimen of infliximab was given at weeks 0, 2 and 6 (Lichtenstein et al., 2005).
For example, Adalimumab is a human immunoglobulin G1 (IgG1) antibody and binds with high affinity and specificity to human soluble TNF (Hanauer et al., 2006). It is effective for inducing of remission and maintaining clinical response in patients with moderate to severe CD. It is approved for the treatment of CD in North America and Europe (Feagan et al., 2008). In the induction therapy of Adalimumab, it was administered subcutaneously as a loading dose at week 0 followed by a second dose at week 2 to CD patients. It resulted in the induction of response and remission in infliximab-native patients with moderate to severe disease activity. The evaluation in its safety and efficacy in long term management of CD patients are currently in clinical trials (Hanauer et al., 2006).
Antibiotics/Fecal transplantation
It is also suggested that the bacteria’s present in intestinal flora also plays an important role in the causing of CD; therefore, antibiotics including metronidazole and ciprofloxacin have been also recommended as an alternative or association with steroids (Scribano and Prantera, 2003). Drugs like sulfasalazine, azathioprine and prednisone have also been used in CD but are having only marginal role in the therapy of acute flare-up of Crohn’s disease (Summers et al., 1979). This strategy is not used anymore.
Fecal microbiota transplantation (FMT) has gained a tremendous interest as a new option for treating IBS. In a study (Colman and Rubin, 2014), 122 patients described as (79 UC, 39 CD and 4 IBD) were treated with FMT. Overall, 45% patients achieved clinical remission from the disease after follow-up. It was suggested that FMT is safe but variably efficacious treatment for IBD.
Table of contents :
1. Synthèse de donneurs de NO
Synthèse de SNOC (S-nitrosoglutathione-oligosaccharides de chitosan)
Synthèse de la SNA (S-nitrosoglutathione-alginate)
2. Microparticules préparées par spray drying : GSH /Eudragit® FS30D et GSNO/Eudragit® FS30D
1. Nitric oxide
Nitric oxide in central nervous system and its action as a neurotransmitter:
Nitric oxide in hypertension
Nitric oxide in immune system
NO and regulation of intestinal function
Nitric oxide and progression of renal disease
Nitric oxide in cancer
Anti-inflammatory effects of NO
2. NO donors
NO donor drugs
Organic nitrates and nitrites
S-nitrosothiols
3. Polymeric carriers for NO
3.1. Micro/nanoparticles
3.2. Thiomers
3.3. Non-biodegradable polymers : Eudragit®
4. Intestine and management of Crohn’s disease
4.1. Small intestine
4.2. Large intestine
4.3. Intestinal barriers to the absorption
5. Crohn’s disease
5.1. Treatment of Crohn’s disease
Objectifs
Results and Discussions
Chapter 1: Synthesis and characterization of S-nitrosoglutathione-oligosaccharide-chitosan as a nitric oxide donor
Chapter 2: Synthesis of S-nitrosoglutathione-alginate for prolonged delivery of nitric oxide in intestines
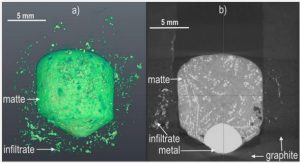
Chapter 3: Spray dried microparticles of glutathione and S-nitrosoglutathione based on Eudragit® FS 30D polymer
Discussion générale (anglais) Conclusion et perspectives (français)
Discussion générale (anglais)
1. Polymer formulations
1.1. Nitrosation of conjugates
1.2. Stability studies
1.3. Permeability studies in the Ussing chamber
1.4. Cytotoxicity studies in the Caco2 cell line
2. GSH and GSNO spray dried microparticles based on Eudragit® FS 30D polymer
2.1. Physical characterization
2.2. In vitro drug release behaviour
2.3. Advantages of spray drying
3. Perspectives
Conclusion et perspectives
References: