Get Complete Project Material File(s) Now! »
ETHICAL CONSIDERATIONS
Approval and ethical clearance
To ensure that the study maintained high ethical standards, a copy of the proposal was submitted and ethical clearance sought from the Health Studies Research and Ethics Committee of the College of Human Sciences, University of South Africa. To ensure that ethical standards of the three countries where the study was conducted were upheld, approval was secured from the National Council for Science and Technology of Kenya, National Institute for Medical Research of Tanzania and Uganda National Council for Science and Technology. In addition, approval was secured from the Research Ethics Committee of the Aga Khan University (AKU) where the researcher works, as is required of faculty working at AKU.Securing approvals from the national councils/institutes in the three East African countries was a long process: it took three months in Kenya, six in Uganda and eight in Tanzania.Whilst the research councils in Kenya and Uganda approved the study with no queries, Tanzania’s institute expressed minor concerns related to language (translating the questionnaire into Kiswahili) and compensation for participants. These concerns were addressed with the National Institute for Medical Research of Tanzania which was informed of the study’s aims and resulting benefits to the participants and of the fact that there was no budget for compensation. The issue of compensation was analyzed and it was felt that if the Tanzania participations were compensated, then they would have felt obliged to participate in the study; furthermore, the information obtained may have been influenced by their perceptions related to compensation received. Additionally, if the Tanzanian participants were compensated, then all the participants would have to be compensated (in terms of the principle of fairness), yet no budget had been allocated for this purpose. Hence, the issue of compensation was dismissed. The Institute in Tanzania was satisfied with the researcher’s response and rationale and granted the research clearance permit. After all approvals were secured, the round 1 questionnaire was pretested.
Ethical principles
The right to autonomy and informed consent was safeguarded by explaining the benefits, rights and risks involved in the research study in writing and securing consent by the return of the questionnaire. A covering letter that explained the purpose of the study at round 1 of the study was attached. Additionally, the researcher’s details were made available to the participants so that they had the opportunity to contact the researcher if they had any questions. They were required to sign the cover page of the questionnaire and return it to the researcher, though returning the questionnaire was also accepted as agreement to partake in the study and implied consent. This was in keeping with the ethical principles of respect and the right of self-determination and of obtaining an informed consent (Burns &Grove 2005:196). The right of self-determination was respected at all times: participants could choose what information they would share with the researcher, and were at liberty to withdraw from the study at anytime without penalty. Informed consent – a covering letter explained the purpose of the study, the type of study and the data collection process as well as requested consent to participate from the expert panellist; it was the first page of the questionnaire (see annexure B). The participants were expected to return a signed consent, although, as indicated, the return of the questionnaire was accepted as consent to participate in the study. Some participants did not return a signed consent but returned a completed questionnaire.Anonymity refers to concealing the identity of the participants in all documents resulting from the research. This meant that the researcher would be unable to identify who returned the questionnaire and who did not; this is a key feature in any survey research. The main advantages were, as mentioned, that it encourages opinions that are true for the individual panellist, and opinions are not influenced by group thinking. Though this may potentially lead to lack of accountability for the response, this is a possibility not unique to a Delphi survey and is true for other self report surveys as well. In a Delphi survey, there is a need to know who has returned the questionnaires and who has not, and this could only be met if the researcher were to be aware of the identity of the individuals.For the purpose of this study, the following principles were applied: The participants expressed their opinions, anonymously.They were anonymous to the group, although the information collected was anonymously shared with the group, which resulted in the collective judgment of experts in the form of group means, standard deviation and percentage agreement (Madigan & Vanderboom 2005:3). This meant that the data was presented in aggregate form, representing the collective views of the expert panel members. Once the questionnaires were returned to the researcher, data entry was undertaken, where each questionnaire was coded; names were not used. The statistical summaries did not encompass the names of the participants or personal details that could link the data to the person. This process continued for 3 rounds. The study endeavoured to ensure anonymity; no panellist or their individual responses was known to anyone other than the researcher and statistician. The returned questionnaires were locked away; only the researcher had access.Confidentiality was maintained at all times throughout the study’s data collection phase and forms were coded numerically. After the data has been analyzed and the study completed to the satisfaction of the University of South Africa, the raw data forms will be destroyed after 3 years.The principle of beneficence is applied to this study, as it is of importance and relevance to nurses and nursing especially in East Africa, where no similar study has been published. This laid the foundation for the ethical premise, as it would have been unethical to carry out a study which would be unlikely to be useful to the profession. From the perspective of health care, patient outcomes and the nursing profession, the researcher’s position is that if health policies are to be geared towards producing the best outcomes, they should be formulated with the aid of input from nurses. The study offers direct benefits to the population being studied. The nurse leaders who participated in the study, and those who did not, will benefit by gaining information related to the extent of nurse leaders participation in health policy development; they will also obtain information related to barriers and facilitators and essential leadership attributes. They may benefit from the recommendations made as a result of the study; if these are implemented, it could help them to influence health policy development. Finally, the empowerment model could provide a framework to enhance their practice in policy development. It is envisioned that the expert panellists will receive the final report of the study. This would be in line with the principle of giving back something to the participants for their time, effort and patience in participating in the study.
Model development
The aim of this study was to develop an empowerment model. A model is a graphic or symbolic representation of phenomena which objectify and present specific perspectives about the nature or function of a phenomenon (McEwen & Wills 2002:27). The empowerment model developed in this study is a theoretical model which was systematically constructed from the findings of scientific inquiry. The literature review lead to identification of the broad concepts related to nurse leaders participation in health policy development. This informed the development of the first questionnaire, which assisted with identifying categories that were linked to the broad concepts. The subsequent questionnaires were iterative and facilitated the gaining of agreement or disagreement on the main concepts and categories. The final questionnaire was further validated by the literature review. The findings lead to the conceptualization of an empowerment model for nurse leaders’ participation in health policy development (discussed in chapter 5). The model was validated by a sample of the panel of experts, who indicated that it represented their ideas. A few minor changes were proposed which were integrated in the final model.
CONCLUSION
The aim of this study was to develop an empowerment model that could be used to enhance nurse leaders’ participation in health policy development. The Delphi survey was applied to gain consensus from a panel of experts (nurse leaders) in East Africa. A purposive sample was drawn from nurse leaders working at national level in Kenya, Tanzania and Uganda. A reiterative questionnaire was utilized for gathering the views of the expert panel, and the study was conducted in three rounds. Statistical analyses were performed to measure the percentage agreement, central tendencies and dispersion.Ethical clearance was secured from various authoritative bodies in the 3 countries and the University through which this doctoral study was done.
FINDINGS AND DISCUSSION
INTRODUCTION
This chapter discusses the findings. This study was conducted by applying the Delphi survey with a group of expert panellists in three iterative rounds, the aim being to develop an empowerment model that could be used to enhance nurse leaders’ participation in health policy development. To achieve this aim, the objectives were to:
– Explore the extent of nurse leaders participation in health policy development in
– East Africa o Build consensus on leadership attributes necessary for nurse leaders’ participation in health policy development in East Africa
– Build consensus on factors that act as facilitators to nurse leaders’ participation in health policy development in East Africa
– Build consensus on factors that act as barriers to nurse leaders’ participation in health policy development in East Africa
– Develop an empowerment model that can enhance nurse leaders’ participation in health policy development
The chapter presents, firstly, a demographic profile of the expert panel members, secondly, reports on the extent of nurse leaders’ participation in health policy development, thirdly, reports the leadership attributes for the said participation, fourthly, presents the facilitators to this participation and finally reports on the barriers in this regard.
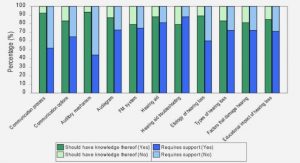
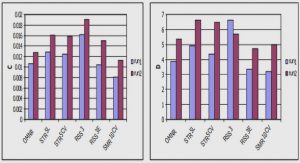
As indicated, from a purposive sample of 78 expert panellists (nurse leaders) in East Africa who were invited to participate, 37 (47.4%) did so in the first round, while of the 37 expert panellists invited to participate in the second round, 24 (64.8%) participated: all 24(100%) participated in the third round. It would appear that by the second round, the expert panellists’ interest in the study had been captured, as all who responded to round 2 continued with round 3. This may suggest that there is a growing interest in the topic among the expert panellists. Considering the iterative nature of the Delphi survey and the sample characteristics (national nurse leaders), the response rate for this study was considered acceptable. Studies utilizing a questionnaire as a data collection tool are known for low response rates (Keeney, Hasson & McKenna 2006:207). Gordon (2009:8) indicates that in his experience, a response rate of 40% to 75% from participants can be expected. During a Delphi survey, the response rates usually decrease with the increasing number of rounds conducted (Van Teijlingen, Pitchforth, Bishop & Russell 2006:249-252). In this study, consensus was built over three rounds. The first round generated unstructured data that is presented in data displays. The second and third rounds gave the expert panellists an opportunity to reevaluate their ideas (consensus building) in line with group summaries and descriptive statistics; these are presented in the tables. The parameters set for round 2 were percentage agreement >=90%and for round 3 were >=70%, a mean value of <2 and standard deviation of <2; these were regarded as convergence of opinion towards agreement and consensus for the purpose of this study. Conversely, a percentage agreement of <90% (2nd round) or <70% (3rd round), mean of >2 and standard deviation of >2 was considered as divergence of opinion. However, if the mean or standard deviation was above the set parameters and the percentage agreement was >=90% (2nd round) and >=70% (3rd round), then the concept was carefully evaluated (see 3.5.4.2). The numbers highlighted in grey indicate the area of lack of consensus.The highlighted areas without numbers (boxes in the table) indicate that the question was not included in that round.
1. OVERVIEW OF THE STUDY
1.1 INTRODUCTION
1.2 BACKGROUND TO THE STUDY
1.3 PROBLEM STATEMENT
1.4 RESEARCH PURPOSE
1.5 RESEARCH OBJECTIVES
1.6 RESEARCH QUESTIONS
1.7 SIGNIFICANCE OF THE STUDY
1.8 DEFINITIONS OF KEY TERMS
1.9 RESEARCH DESIGN AND METHODS
1.10 SCOPE OF THE STUDY
1.11 ORGANISATION OF THESIS
2. LITERATURE REVIEW
2.1 INTRODUCTION
2.2 POLICY DEVELOPMENT
2.3 INVOLVEMENT OF NURSES IN HEALTH POLICY DEVELOPMENT
2.4 BARRIERS TO NURSES’ INVOLVEMENT IN HEALTH POLICY DEVELOPMENT
2.5 FACILITATORS OF NURSES’ INVOLVEMENT IN HEALTH POLICY DEVELOPMENT
2.6 NURSING LEADERSHIP
2.7 EMPOWERMENT
2.8 SUMMARY
3. RESEARCH DESIGN AND METHODOLOGY
3.1 INTRODUCTION
3.2 RESEARCH DESIGN
3.3 PHILOSOPHICAL ORIENTATION
3.4 APPLICATION OF THE DELPHI SURVEY
3.5 DATA COLLECTION PROCESS AND ANALYSIS
3.6 ETHICAL CONSIDERATIONS
3.7 CONCLUSION
4. FINDINGS AND DISCUSSION
4.1 INTRODUCTION
4.2 DEMOGRAPHIC DATA
4.3 EXTENT OF NURSE LEADERS’ PARTICIPATION IN HEALTH POLICY DEVELOPMENT
4.4 LEADERSHIP ATTRIBUTES FOR NURSE LEADERS’ PARTICIPATION IN HEALTH POLICY DEVELOPMENT
4.5 FACILITATORS TO NURSE LEADERS’ PARTICIPATION IN HEALTH POLICY DEVELOPMENT
4.6 BARRIERS TO NURSE LEADERS’ PARTICIPATION IN HEALTH POLICY DEVELOPMENT
4.7 SUMMARY
5. EMPOWERMENT MODEL FOR NURSE LEADERS’ PARTICIPATION IN HEALTH POLICY DEVELOPMENT
5.1 INTRODUCTION
5.2 BACKGROUND TO THE MODEL
5.3 ASSUMPTIONS OF THE MODEL
5.4 DESCRIPTION OF THE MODEL
5.5 VISUAL PRESENTATION OF THE EMPOWERMENT MODEL FOR NURSE LEADERS’ PARTICIPATION IN HEALTH POLICY DEVELOPMENT
GET THE COMPLETE PROJECT
AN EMPOWERMENT MODEL FOR NURSE LEADERS’ PARTICIPATION IN HEALTH POLICY DEVELOPMENT