Get Complete Project Material File(s) Now! »
THE IMPACT OF INFECTIOUS DISEASES
Infectious diseases are important in public health for communities in Africa and the developing world (Sparg et al., 2000). These diseases, and subsequent deaths, have devastating consequences for developing economies. Meagre health budgets and lack of adequate medical facilities hinder efforts by poor African countries to match the overwhelming treatment and prevention burden presented by these diseases (Louw et al., 2002).
A diverse range of diseases afflicts people and animals worldwide. Over 200 million people in many countries are infected with Schistosomiasis, while a further 500-600 million (4.5% of the world’s population) are at risk of being infected (Basch, 1991). Sexually transmitted diseases (STD’s), including HIV/AIDS are a major public challenge in most African countries (Green, 1992; Ndubani, 1999). In sub-Saharan Africa, communicable diseases account for more than 70% of the burden of ill health as compared to about 10% in developed countries (World Bank, 1997).
In South Africa, outbreaks of cholera and typhoid (Sidley, 2005) have been reported in recent times. In 2005 alone, Sidley (2005) reported that 14 000 people in rural parts of the KwaZulu-Natal province of South Africa contracted cholera and that 50 people died allegedly due to the outbreak. About 18 million South Africans in rural areas do not have access to clean running water, toilets and adequate sanitation, further increasing the risk of contracting cholera. Pneumonia, especially in alcoholics, continues to be an important community-acquired infection (Ko et al., 2002). Some hospitals in South Africa have been ravaged by Klebsiella. In Durban’s Mahatma Gandhi Memorial Hospital in 2005, 110 babies died allegedly as a result of Klebsiella infections between 2004 and 2006 (Cullinan, 2006).
Western or modern medicine has for many years been used, with varying degrees of success, in the treatment of infectious diseases. Furthermore, improved sanitation, clean water, better living conditions and vaccines brought many infectious diseases under control (Wilson, 1995). Despite this, many obligate and opportunistic pathogens are becoming increasingly resistant to most available drugs at an alarming rate that is unmatched by the development of new drugs (Neu, 1992).
In South Africa HIV/AIDS problems continue to ravage the communities, leading to high levels of opportunistic infections, manifesting as the so-called AIDS-related symptoms. Among the opportunistic infections in immunocompromised patients is candidosis, commonly caused by Candida albicans.
CANDIDOSIS
Candida albicans, which accounts for more than 80% of candidosis cases, is a member of the commensal flora of the gastrointestinal and genitourinary tract of dogs, cats and humans (Greene & Chandler, 1998). This microorganism exists in a variety of morphological forms, ranging from unicellular budding yeast to true hyphae (Sudbery et al., 2004). The morphology is dependent on cell density, nutrient availability and pH of the environment (Sudbery et al., 2004).
Candida albicans is considered to be an opportunistic pathogen in these species, able to access different locations of the body, causing disease when the host defense is compromised (Kobayashi and Cutler, 1998). Candidal urinary infections in dogs are associated with cystic calculus (Tan & Lim, 1977), hypothyroidism and diabetes mellitus (Forward et al., 2002). In cats infections with Candida are reported with perineal urethrostomy (Fulton & Walker, 1992), diabetes mellitus and urinary tract infection (Marshall et al., 2002) and hyperadrenocorticism (Gerding et al., 1994). Pressler et al. (2003) reported the observation of C. albicans and other non-albicans strains in 62% of dogs and 43% of the cats in a study to evaluate urinary tract infection in these animals.
albicans causes vaginitis in otherwise healthy women, severe surface infections of the mouth and the esophagus in human immunodeficiency virus (HIV) patients and blood stream infections in vulnerable intensive care patients (Kao et al., 1999). Vaginal candidosis, resulting from infection with C. albicans and C. vaginitis, is a common condition that affects approximately 75% of women at least once in their lifetime. C. albicans is the most common cause of vaginal candidosis, accounting for over 80% of The combination of microbial virulence, environmental influences and host defense factors determine the progression of candidosis and various manifestations that accompany the infection.
Predisposing factors to candidosis
Environmental conditions such as pH and temperature changes trigger dimorphism, which allows C. albicans to switch from unicellular to hyphal growth. Dimorphism permits the organism to invade tissues and thus, contributes to the virulence of this microorganism (Ryley & Ryley, 1996; Magee, 1998; Corner and Magee, 1997). Reduced salivary flow, epithelial changes, changes in commensal flora, and a high carbohydrate diet have been observed as local factors predisposing humans to oral candidosis (Farah et al., 2000). A variety of nutritional factors that include deficiencies of iron, folic acid and vitamins have also been linked with candidosis (Cawson, 1966; Higgs and Wells, 1972). Diabetes, hypothyroidism, hyperparathyroidism and adrenal suppression resulting from an altered hormone state, have also been implicated in progression of candidosis, provided there is a preceding immune system defect (Kostiala et al., 1979).
CHAPTER 1
1 INTRODUCTION
1.1. THE IMPACT OF INFECTIOUS DISEASES
1.2. CANDIDOSIS
1.2.1. Predisposing factors to candidosis
1.2.2. Immunodeficiency and candidosis
1.2.3. Pathogenesis
1.2.3.1. Adhesion
1.2.3.2. Epithelium invasion
1.2.4. Treatment
1.2.4.1. Polyenes
1.2.4.2. 5-Flucytosine
1.2.4.3. Azoles
1.3. MEDICINAL PLANTS
1.3.1. Overview
1.3.2. Isolation of Compounds from Medicinal Plant Species
1.3.3. Some compounds isolated from plants
1.3.3.1. Phenolic compounds
1.3.3.2. Terpenoids
1.3.3.3. Essential oils
1.3.4. Ethnobotany and Drug Discovery
1.3.5. Determination of Biological Activities of Medicinal Plants
1.4. PLANTS USED IN THE STUDY
1.4.1. Curtisia dentata (Burm. f) C.A. Sm
1.4.2. Trichilia emetica Vahl
1.4.3. Kigelia africana (Lam.) Benth
1.4.4. Cussonia zuluensis Strey
1.4.5. Terminalia phanerophlebia Engl. & Diels
1.4.6. Terminalia sambesiaca Engl. & Diels
1.4.7. Vepris reflexa I. Verd
1.5. SUMMARY AND PROBLEM STATEMENTS
1.6. HYPOTHESIS
1.7. AIM OF THE STUDY
1.8. OBJECTIVES OF THE STUDY
CHAPTER 2 GENERAL MATERIALS AND METHODS
2.1. REVIEW OF GENERAL METHODS
2.1.1. Selection of plant species 29
2.1.2. Extraction
2.2. PROCESSING OF PLANT MATERIAL
2.2.1. Plant Collection and storage
2.2.2. Preliminary extraction for screening
2.2.3. Serial Exhaustive Extraction
2.2.4. Thin Layer Chromatography (TLC)
2.3. BIOLOGICAL ACTIVITY METHODS
2.3.1. Fungal cultures
2.3.2. Bacterial cultures
2.3.3. Bioautography Procedure
2.3.4. Minimal Inhibitory Concentration Determination
2.3.5. Cytotoxicity
2.4. BIOASSAY-GUIDED FRACTIONATION
2.5. STRUCTURE ELUCIDATION
CHAPTER 3 PRELIMINARY SCREENING
3.1. MATERIALS AND METHODS
3.1.1. Extraction
3.1.2. Test Organisms
3.1.3. Bioautography of extracts
3.1.4. Minimal Inhibitory Concentration Determination
3.1.5. Cytotoxicity and selectivity index
3.2. RESULTS
3.2.1. Mass extracted from leaves
3.2.2. Antifungal activity of extracts of the leaves
3.2.2.1. Bioautography
3.2.2.2. Minimal Inhibitory Concentrations against fungi
3.2.3. Antibacterial activity of extracts of the leaves
3.2.3.1. Bioautography
3.2.3.2. MIC values against bacteria
3.2.4. Cytotoxicity of acetone and dichloromethane extracts of C. dentata
3.3. Comparison of antifungal and antibacterial activity of stem bark and leaves of Curtisia dentata
3.3.1. TLC fingerprints
3.3.2. Comparative bioautography
3.3.3. Minimal inhibitory concentrations
3.4. DISCUSSION
3.5. CONCLUSIONS
CHAPTER 4 ISOLATION OF ACTIVE COMPOUNDS FROM C. dentata (Burm.f) C.A. Sm.
4.1. INTRODUCTION
4.1.1. Compounds isolated from Cornaceae family
4.2. MATERIALS AND METHODS
4.2.1. General Methods
4.2.1.1. Plant Part Collection
4.2.1.2. Serial exhaustive fractionation
4.2.2. Overview of approach followed
4.2.2.1. Selection of stationary phase
4.2.2.2. Group separation (column I)
4.2.2.3. Combination of fractions from column I (DCM extract)
4.2.2.4. Isolation of compound CI (column II)
4.2.2.5. Isolation of compound CII and CIII (column III)
4.2.2.6. Isolation of compound CIV (column IV)
4.2.2.7. Isolation of compound HI (column V)
4.3. RESULTS
4.3.1. Serial exhaustive extraction
4.3.2. Activity of serial exhaustive extraction samples
4.3.2.1. Anti-Candida activity
4.3.2.2. Antibacterial activity
4.3.3. Isolation of compounds
4.4. DISCUSSION
4.4.1. Serial Exhaustive Extraction of C. dentata Leaves
4.4.2. Isolation of compounds
4.5. CONCLUSIONS
CHAPTER 5 STRUCTURE ELUCIDATION
5.1. INTRODUCTION
5.2. MATERIALS AND METHODS
5.2.1. Thin layer chromatography
5.2.2. 13C and 1H NMR spectroscopic analysis
5.2.3. Mass Spectrometry
5.3. RESULTS AND DISCUSSION
5.3.1. Thin Layer Chromatographic Analysis of Isolated Compounds
5.3.2. Characterization of compound CI
5.3.3. Characterization of compound CII
5.3.4. Compound CIII
5.3.5. Compound CIV
5.3.6. Estimation of betulinic acid content of C. dentata leaves
CHAPTER 6 ANTIMICROBIAL ACTIVITY OF ISOLATED COMPOUNDS
6.1. INTRODUCTION
6.2. MATERIALS AND METHODS
6.2.1. Bioautography
6.2.2. Minimal Inhibitory Concentration (MIC) Determination
6.2.3. Cytotoxicity
6.3. RESULTS
6.3.1. Antifungal activity
6.3.2. Antibacterial Activity
6.3.3. Cytotoxicity
6.4. DISCUSSION
6.4.1. Lupeol and betulinic acid
6.4.2. Ursolic acid and Hydroxyursolic acid
6.4.3. Cytotoxicity
6.5. CONCLUSIONS
CHAPTER 7 IN VIVO ANTIFUNGAL AND WOUND HEALING ACTIVITY OF CURTISIA DENTATA EXTRACTS, LUPEOL AND BETULINIC ACID
7.1. BACKGROUND
7.2. MATERIALS AND METHODS
7.2.1. Rats
7.2.2. Housing and feeding conditions
7.2.3. Preparation of animals
7.2.4. Wound creation
7.2.5. Infection with C. albicans
7.2.6. Preparation of extracts
7.2.7. Observations
7.2.8. Evaluation of lesions
7.2.9. Recording of data
7.2.10. Statistical analysis
7.2.11. Pathological and histopathological studies
7.3. RESULTS
7.4. DISCUSSION AND CONCLUSIONS
7.4.1. Weight loss and temperature
7.4.2. Lesion sizes
7.4.3. Exudate and erythema
7.4.4. Presence of infection on skin and internal organs
CHAPTER 8 ANTIHELMINTIC ACTIVITY OF CURTISIA DENTATA EXTRACTS, LUPEOL, URSOLIC ACID AND BETULINIC ACID
8.1. INTRODUCTION
8.2. MATERIALS AND METHODS
8.2.1. Plant extracts and compounds
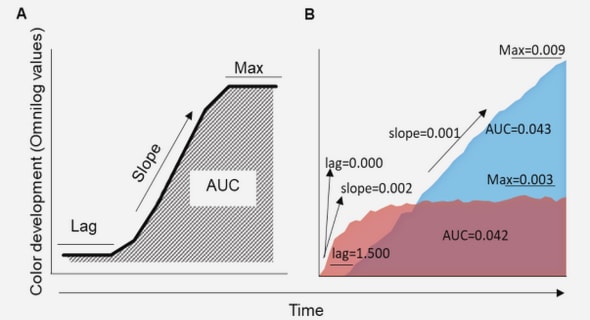
8.2.2. Anthelminthic activity
8.2.2.1. Recovery and preparation of eggs
8.2.2.2. Egg hatch inhibition assay
8.2.2.3. Anthelminthic activity against L3 stage larvae
8.2.2.4. Anthelminthic activity against developing larvae
8.2.2.5. C. elegans
8.2.2.6. Calculation of LC50 values
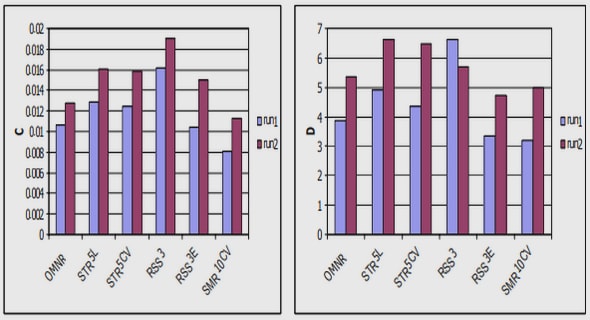
8.3. RESULTS
8.3.1. Egg hatching
8.3.2. Inhibition of motility of adult parasitic nematodes
8.3.3. Inhibition of motility of free-living nematodes
8.4. DISCUSSION AND COCLUSION
CHAPTER 9 GENERAL DISCUSSIONS AND CONCLUSIONS
9.1. ANTIFUNGAL AND ANTIBACTERIAL ACTIVITY OF SELECTED PLANT SPECIES
9.2. SELECTION OF THE MOST PROMISING TREE SPECIES FOR ISOLATION OF ACTIVE COMPOUNDS
9.3. ISOLATED COMPOUNDS
9.4. ANTHELMINTHIC ACTIVITY
9.5. CYTOTOXICITY
9.6. IN VIVO STUDIES
9.7. CONCLUSIONS
CHAPTER 10
REFERENCE
APPENDIX