Get Complete Project Material File(s) Now! »
Cell-attachment treatment
When serum-free media are used for cell culture, even treated polystyrene cannot be used since there is no more serum protein deposition. Then, BM proteins were considered for surface coating of the substrate to improve the cell attachment, migration, and function [164]. In addition, mucopolysaccharides such as heparin sulfate, hyaluronic acid, and chondroitin sulfate, and synthetic polymers such as poly-D-lysine (PDL) are used for coatings to generate a positively charged surface of polystyrene. For certain cell types, it can enhance cell attachment, growth, and differentiation, especially in serum-free and low serum conditions. PDL coating can generally improve the attachment and growth of primary neurons, glial cells, neuroblastoma, and various transfected cell lines [165]. Inspired by this, nanofiber substrates using these coatings are more suitable for growing cells under serum-free conditions and maintaining primary cell cultures.
Ultra-Low attachment treatment
Sometimes there is a need to prevent the cell from attaching to a surface. Although untreated polystyrene surfaces are hydrophobic, certain cell types can still attach to it, due partially to their sterilization by irradiation. In order to minimize cell adhesion, Corning® introduced ultra-low adhesion surface coating containers in the 1990s. These containers have a very hydrophilic and neutrally charged hydrogel layer that is directly covalently attached to the polystyrene surface to prevent peeling. Because cell attachment proteins and other biological molecules are passively adsorbed to the polystyrene surface through hydrophobic or ionic interactions, the hydrogel surface naturally inhibits non-specific immobilization through these interactions, thereby inhibiting subsequent cell attachment. The surface is very stable, non-cytotoxic, and biologically inert.
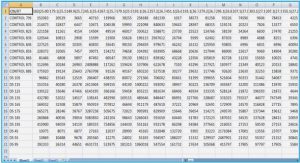
Figure 1.8 Formation of 3D microtissues on ultra-low attachment plate or after hanging drop transfer. Better image quality can be achieved for those on ultra-low attachment plates.
The ultra-low attachment surface can be used to prevent attachment and activation of macrophages and neutrophils [166]. It can also be used for spheroid and tumoroid formation (see Fig 1.8), which in turn allows isolating both primary tumor and stem cell spheroids from the brain and mammary tissues [167-171], and can help avoid overgrowth by normal cells which will undergo apoptosis. The ultra-low attachment surface is also recommended for easy-to-harvest embryoid bodies derived from embryonic stem cells or induced pluripotent stem cells [172].
Besides, lab-made ultra-low attachment substrates also hold good quality based on commercial Petri dishes and multi-well plates or the formation of hydrogel multiwells. Agarose is an ideal polysaccharide which inhibits cell attachment and promotes cell aggregation due to the linear molecule structure. In laboratory studies, low attachment surfaces are usually formed by applying a thin layer of agarose gel on Petri dishes or multi-well plates. Uniform tumor spheroids and embryoid bodies can be also easily harvested via cell seeding on this hydrogel surface [173, 174]. Moreover, nanofiber-based bioscaffolds can be also coated with a thin layer of gel to form a low-attachment 3D culture substrate.
From 2D to 3D culture substrate
For many years, culturing cells in Petri dishes and tissue culture flasks (i.e. in vitro) has experienced a completely different microenvironment compared with the natural tissues in the complex three-dimensional extracellular matrix (in vivo), resulting in the various cell morphology and functions. Compared with the current in vivo research, the miniaturized microfluidic culture system (in vitro) can have more advanced tissue functions [175, 176]. Compared to any current in vitro models, this allows for more precise studies of the complex mechanisms of tissue growth, renewal and disease without the difficulties inherent in in vivo studies.
Nowadays, there are many models available for cell culture, namely: 2D or 3D static cell culture and 2D or 3D perfusion microfluidic cell culture. From 2D to 3D culture, cell growth behavior has undergone many changes, from cell shape and structure to cell-cell adhesion tissue, mainly due to differences in cell microenvironment. Clearly, in vitro 3D culture can better simulate the in vivo condition of cells in organs and tissues. Compared with 3D static culture, microfluidic-assisted 3D culture can better deal with related topics, such as multi-cell complex environments, cell vascularization, and continuous medium exchange instead of discrete exchange [177-179]. Besides, several parameters of the sample (such as pH, oxygen, CO2, temperature, osmotic pressure, shear stress) need to be monitored for further downstream studies. All these issues make the 3D culture as close as possible to the internal organs. Recently, many efforts in microfluidic 3D cell culture have targeted lung, vessel, brain, and liver models, or improved cancer models [180-182]. These studies have a crucial impact on understanding the basis of cell activity, which plays a key role in determining physiological and pathological cell states (such as disease characteristics and response to stimuli). The main goal of the cell culture platform is to closely simulate the cell microenvironment in the body and maintain simplicity to obtain reproducible results.
Air-liquid interface
Many cells can be used to model the human respiratory system, including immortalized respiratory cell lines (i.e., A549 cells), primary cells from animals or human donors, and alveolar or airway epithelial cells derived from hiPSCs [183-186]. Although immortalized cell lines and primary cells from animals are widely used, data generated using these cells are not applicable to humans. Submerged culture of primary human alveolar or airway epithelial cells is possible; however, cells in this system fail to undergo further differentiation. In order to recapitulate the phenotype observed in vivo, primary human alveolar or airway epithelial cells must be cultured at an air-liquid interface (ALI) as shown in Fig 1.9.
Cell culture at the air-liquid interface (ALI) is necessary for respiratory research since submerge culture is not applicable. ALI culture of alveolar epithelial cells can be used, for instance to:
A. Study the cell biology of the respiratory epithelium, since it is most physiologically relevant for in vitro modeling of the respiratory epithelium [187-189].
B. Study respiratory diseases. Alveolar epithelial cells from patients with chronic respiratory diseases such as cystic fibrosis, chronic obstructive pulmonary disease (COPD) and asthma, can be cultured using ALI techniques, enabling disease mechanisms to be studied in vitro.
C. Study infection of the respiratory epithelium. Some respiratory viruses selectively target cell types present only in fully differentiated alveolar cell cultures, such as the novel coronavirus SARS-CoV-2 binding to the angiotensin-converting enzyme 2 (ACE2) on alveolar epithelial cells [190-192].
D. Test drugs for inhalation delivery. Aerosol particles can be directly deposited onto the semi-dry apical cell surface, mimicking the deposition of powders onto the lung surface in vivo.
E. Test toxicity of inhaled substances. Responses of ALI-differentiated primary epithelial cells to insults such as tobacco smoke components closely mimic reported changes in the human alveoli [193, 194].
Microfluidic technologies
Microfluidic technologies can control a small volume of fluids (from microliters to picoliters) inside micrometer-level channels, which are increasingly used in various tissue engineering applications, such as bioreactor perfusion, cell patterning, and droplet-based fabrication of biomaterials.
Table of contents :
Chapter 1 Introduction
1.1 Cells and stem cells
1.1.1 Cells
1.1.2 Stem cells
1.1.3 Induced pluripotent stem cell
1.2 Cellular microenvironment
1.2.1 ECM
1.2.2 Soluble factors
1.2.3 Cell-cell contact
1.3 Physiological systems
1.3.1 General notions
1.3.2 Lung and alveoli
1.4 Cell culture substrate
1.4.1 Hydrogels
1.4.2 Nanofibers
1.4.3 Surface treatment
1.4.3.1 Cell-attachment treatment
1.4.3.2 Ultra-Low attachment treatment
1.4.4 From 2D to 3D culture substrate
1.4.5 Air-liquid interface
1.5 Microfluidic technologies
1.5.1 Introduction of microfluidic device
1.5.2 Fabrication methods of microfluidic device
1.5.2.1 Lamination
1.5.2.2 Molding
1.5.2.3 3D printing
1.6 Cell-based assays
1.6.1 Organ-on-a-chip
1.6.1.1 Lung-on-a-chip
1.6.1.2 Liver-on-a-chip
1.6.1.3 Kidney-on-a-chip
1.6.1.4 Gut-on-a-chip
1.6.1.5 Heart-on-a-chip
1.6.1.6 Multi-organ-on-a-chip
References
Chapter 2 Device fabrication and microfluidic techniques
2.1 Photolithography
2.2 Vacuum-assisted molding
2.2.1 PDMS mold fabrication
2.2.2 PEGDA molding
2.3 Electrospinning
2.3.1 Electrospinning
2.3.2 Chemical crosslinking
2.3.3 Thermal crosslinking
2.4 Micro-milling
2.5 Cutting plotter
2.6 Parylene deposition
2.7 Culture patch, basement membrane mimics and accessories
2.7.1 Culture patch
2.7.2 Ultrathin artificial basement membrane
2.7.3 Chamber for improved cell seeding on patch
2.7.4 Patch handler for Air-liquid interface (ALI) culture
2.8 Microfluidic devices
2.8.1 Device configuration
2.8.2 Mechanical clamping
2.8.3 Concluding remarks
References
Chapter 3 Automatic stem cell differentiation
3.1 Introduction
3.2 Development of the system
3.3 Dynamic cell culture
3.4 Cardiac differentiation
3.4.1 Fabrication of the culture patch
3.4.2 Preparation of the culture media with different factors
3.4.3 Protocol implementation
3.4.4 Results
3.5 Neuron network maturation
3.5.1 Protocol implementation
3.5.2 Operation details
3.5.3 Results
3.6 Conclusion and discussions
References
Chapter 4 Fabrication of alveolar tissue constructs
4.1 Introduction
4.2 Fabrication of alveolar organoids
4.2.1 Preparation of medium and soluble factors
4.2.2 HiPSCs maintenance
4.2.3 Definitive endoderm
4.2.4 Anterior foregut endoderm
4.2.5 Bud tip progenitor organoids
4.2.6 Maturation of alveolar organoids
4.3 Manipulation of alveolar organoid
4.3.1 Passage of alveolar organoids
4.3.2 Cryopreservation of alveolar organoids
4.3.3 Thawing of alveolar organoids
4.3.4 Dissociation and replating
4.3.5 Air-liquid interface (ALI) culture
4.4 Characterization of alveolar organoids and derived epithelium
4.4.1 Immunocytochemistry
4.4.2 TEER monitoring
4.5 Conclusion
References
Chapter 5 Response of hiPSC derived cells to S-proteins of SARS-CoV-2
5.1 SARS-CoV-2: Physiological aspects
5.2 SARS-CoV-2: Virus-host interaction
5.3 ACE2 and renin-angiotensin system
5.4 Effect of S-protein
5.5 ROS monitoring
5.6 Response of iPSC derived cardiomyocytes
5.7 Discussion
5.8 Conclusion
References
Chapter 6 Conclusion and perspectives