Get Complete Project Material File(s) Now! »
Patient Identification Systems
This chapter gives a general overview of the different technologies that can be used for patient identification applications in hospitals. It briefly compares these systems in terms of the technology used, limitations, and benefits of each approach with respect to positive patient identification at the point of care1. This chapter also briefly covers topics on patient safety, patient identifier schemes, patient privacy, from the point of view of patient identification.
Patient Safety at the Point of Care
Accurate information about the patient at the point of care is critical to the successful delivery of medication and care to patients in hospitals. In 2001, the U.S. National Institute of Medicine issued an important report titled: “To Err Is Human, Building a Safer Health System”, which described the prevalence and widespread problem of medical errors (which are often preventable) throughout hospitals in the United States. The report highlighted that preventable medical errors cause up to 98,000 deaths and 770,000 adverse drug events2 in the U.S. each year [37]. These are remarkable figures considering that the U.S. has highest expenditure for healthcare of any country in the world [11].
Similar studies in Europe confirm that medical errors are on the increase [44] and subsequent figures published by the U.S. Joint Commission on Accreditation of Healthcare Organisations (JCAHO) have revealed that the problem not only persists, but it appears to be escalating [33].
It was identified in each of these studies, that a large majority of the medical errors were attributed to adverse drug events, specimen misidentification, and incorrect blood transfusions; caused primarily by incorrect identification (direct or indirect) of the receiving individuals [66].
Despite the evidence that medical errors are a persistent and growing problem in many hospitals, very little has been done to reverse the trend [29]. Industry efforts to address patient safety and patient misidentification are mainly focused on error reduction at the point of care usually through technological solutions such as barcode or radio frequency identification [50].
Overview of Patient Identification Systems
Barcode Identification
A barcode is a machine readable representation of encoded information usually printed on a surface in the form of a pattern3. Initially, barcodes could only store limited information in the widths and spacings of printed parallel dark lines (traditional barcode – see figure 2.1) but with recent technology improvements, barcodes can now be printed in patterns of dots, sequential lines, and two-dimensional images and are able to store up to two-thousand text characters (see figure 2.1). In healthcare applications, barcode solutions have proven to be effective in reducing patient misidentification, blood transfusion errors, and drug administration errors [2], as part of improving patient safety in hospitals [21].
For instance, in a medication administration application, barcode solutions often include a barcoded wristband issued to the patient at the time of admission (as shown in figure 2.2). Similarly, staff ID badges and medications may also have barcodes printed on them. Usually, when a medication is administered, all the relevant barcodes would be scanned at the bedside, this includes: the patient’s barcode wristband, the nurse’s ID badge, and the medication’s barcode. This assures a match between the patient and the medication, and also identifies the physician or nurse administering the medication for compliance with the “Five rights” of patient medication administration4 [52].
For patient identification applications, barcodes are primarily used to record demographic information about patients5. This barcode information is usually stored using a barcoded wristband which then serves as an index-key to the patient’s medical information on the hospital information system (HIS) or the different clinical systems in the hospital, as shown in figure 2.26.
In other clinical applications, hospitals usually deploy barcoding solutions for tagging unlabelled unit-of-use medications, to manage clinical inventory and assets, and to record medical interventions for each patient receiving medications or blood transfusions [20]. Similarly, pharmacies in hospitals use barcoding to update and audit their drug inventory and automate record keeping of pharmaceuticals used in the hospital [35].
Challenges of barcode technology in healthcare
Quality of the barcodes and durability
A key requirement of bar coding for healthcare is clarity and definition of the barcode in labels and wristbands. As barcodes become smaller (in order to accommodate more data), the need for readability and precision increases. Edge definition, which refers to the clarity and contrast of the dark and light edges within a barcode symbol, is a problem with ink jet and laser barcode printers and may cause a printed barcode to be prone to misreads. In addition, ink jet and laser printers may require higher quality ink or toner otherwise there may be undesirable degradation over time in the quality of printed labels and barcodes.
Price of the technology
Some hospitals still find barcode technology solutions expensive, since the implications for using barcode in healthcare scenarios usually requires the integration of software, printers, and other barcode equipment with the existing clinical systems at the hospital, and depending on the sophistication of the hospital’s IT systems this could be a lengthy, expensive, and complex task.
Lack of industry standards and regulations
At present there is no single industry standard regulating the use of barcodes in hospitals and what information should be encoded onto them. In recent years, the U.S. Food and Drug administration has proposed several regulations regarding the use of barcode in American hospitals, but worldwide there are still some significant challenges to the adoption of barcode technologies in healthcare, additionally each hospital usually has different needs. The fact that there are over 200 barcode symbologies and several of them are being considered for use in healthcare applications is an example of this. In addition, it is common to find that medical departments in hospitals have implemented different barcode solutions which are often incompatible with the barcode systems in other departments (e.g. blood bank barcode label is not compatible with laboratory label) this may cause a patient to wear several barcode wristbands or labels7 at the same time.
Functional limitations of barcode technology
A limitation of barcode is that it can not update information in real-time, once a barcode is printed, the information on it remains fixed and can only be changed by re-printing the barcode. The initial concept of a barcode was intended to operate in this way.
Integration and interoperability
A common impediment to the use of barcode technology in hospitals is due to vendor-lock in8 issue created by companies supplying barcode solutions. Thus if a hospital has already deployed a barcode solution and desires to enhance or change some functionality of their systems using barcode solutions from another vendor, it may prove difficult due to the a single vendor approach and the vendor-lock in of some barcode products. Integration of multiple barcode products is often difficult because the ownership of barcode systems remains in hands of the barcode companies, not the hospitals.
Radio Frequency Identification
The term radio frequency identification (RFID) describes a wireless identi-fication technology that communicates data by using radio waves9. Data is encoded in a chip, which is integrated with an antenna and packaged into a finished label or tag, as shown in figure 2.310 (a) and (d). RFID tags (also called transponders) may be passive (requiring close proximity to a RFID reader11), or active, in which case the RFID tag contains a small battery to allow continuous monitoring (used mostly to track equipment and for long range applications).
RFID technologies offer different rewritability options, memory sizes, and tag forms, and can be read from anywhere within range of the RFID reader. Some RFID labels can hold more data than barcodes, and can be read automatically without any user intervention required.
RFID in healthcare applications
At present, the application of RFID technology in hospitals has been modest, mainly due to the cost of the technology. Like most electronic technologies, RFID unit costs have fallen dramatically within the past few years, but have not yet achieved the tipping point of economic viability for cost conscious hospitals. In practical healthcare applications, RFID has been primarily restricted to asset management of documents and medical equipment, patient identification, and other specific applications.
Similar to barcode applications in healthcare, RFID has found intriguing applications for improving the delivery of healthcare and welfare of patients in hospitals. For instance, typical RFID applications in hospitals include:
Improvement of legacy barcode applications using RFID, i.e. blood transfusion, pharmaceutical tracking, and specimen identification.
Applications to track long-term care elderly or disoriented patients [48]. Applications for surgical patients who can be tagged to ensure that the right procedure is being performed on the right person at the right time [67].
Positive patient identification applications using a smart patient wrist-band that when scanned by a RFID reader reveals patient name, date of birth, admitting orders, insurance information, surgical site, allergic reactions, medication requirements, and blood type. See figure 2.3 (b) and (c).
Applications for tracking and monitoring surgical equipment before and after operations [12].
Applications using implantable RFID devices that act as a portable medical record for patients, see figure 2.3 (e).
Applications for tracking doctors, nurses, and patients anywhere in a hospital by using RFID enabled badges and ID cards, see figure 2.3 (f).
Existing RFID handheld identification systems
Today, there are many RFID readers available in the market for different applications. However, for healthcare applications, features such as: wireless connectivity, barcode support, long battery operation, and multi-tag stan-dard support, must be considered as important requirements.
Precision Dynamics Corporation Feig Tethered Reader R110-00-PDA
The R110-00-PDA (as shown in figure 2.4-a) is a tethered 13.56 MHz RFID reader and writer for connection to computers or other data terminals via a RS-232 serial port. This handheld reader is able to identify any transponder simultaneously which follows the ISO-15693 standard13, e.g. Tag-it, I-Code, my-d, and STM.
Precision Dynamics Corporation DR1000 Dual Reader
DR1000 Dual Reader (as shown in figure 2.4-b) is a dual RFID and barcode and can read and write to any tags and smart labels compliant with the ISO-15693 industry standard at 13.56 MHz. It provides an easy migration path from barcodes to RFID tags. The reader has no external graphical user interface, but this functionality can be provided by a desktop PC, laptop, or PDA using a RS-232 serial port.
Precision Dynamics Corporation TEK RFID Reader P103-00- PDA
The TEK P103-00-PDA RFID Reader/Writer (as shown in figure 2.4- c) includes a Palm i705 personal digital assistant device to read and write information to RFID wristbands and labels using an operating frequency of 13.56 MHz . The reader is ISO 15693-1, 2, and 3
compatible and includes a demo program for RFID wristbands. Symbol Technologies MC9000-G RFID Reader
The MC9000-G RFID Reader from Symbol Technologies (as shown in figure 2.4-d) is a ruggedized mobile computer that features integrated support for the most popular radio frequency identification standards. This device combines RFID and barcode reading and also has IEEE 802.11b wireless network connectivity, along with a full 1/4 VGA screen and alphanumeric keypad. The software interface for the reader is
based on the Windows Mobile 2003 operating system.
Socket Communications Compact Flash RFID Reader Card 6E
This Compact Flash RFID reader from Socket Communications (see figure 2.4-e) reads and writes to any ISO-15693 and other proprietary 13.56Mhz RFID tags. The reader can be used for asset tracking, access control, and process control – in healthcare, medical, and pharmaceutical applications. This reader has the advantage that it can interface to any commercial handheld equipped with a compact flash connector. The reader comes with an easy to use software wedge
interface for scanning RFID tags.
Cathexis Innovations Bluetooth RFID reader
This light weight RFID bluetooth reader from Cathexis Innovations (see figure 2.4-f), features RFID functionality along with Bluetooth connectivity. The reader aims to replace the typical bulky and cumbersome RFID readers that may not be suitable for medical personnel to carry around. The Bluetooth connectivity of the reader allows it to share RFID tag information with other systems, e.g. Bluetooth equipped handhelds, desktops, and laptops, allowing the reader to be de-coupled from a particular hardware and software implementation. This type of reader may be particularly advantageous in hospitals where the staff already carry PDAs with Bluetooth and WLAN interfaces.
For a more detailed overview of the features and applications of the RFID readers, see [59].
Comparison of Barcode and RFID
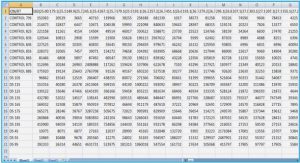
The use of RFID technology can substitute barcode solutions in hospitals, but its use so far has been limited to applications where the use of barcode technology is not adequate, e.g. patient tracking applications. RFID overcomes some of the limitations of barcode technology, but at some cost. Table 2.1 illustrates some of the differences between barcode technology and radio frequency identification technology.
It is likely that in the future, barcode solutions and RFID will complement each other in terms of functionality, cost, and usability. Today, hospitals are reluctant to abandon their initial investments in barcode systems simply to introduce technology replacements. As RFID technology matures, the use of RFID will continue to grow in healthcare, particularly via asset and inventory management applications, then it will move towards personnel and patient identification, and tracking of clinical devices and pharmaceuticals.
Challenges of RFID technology in healthcare
Quality of RFID tags and reliability
For positive patient identification applications in hospitals, RFID technology inherits some of the challanges of barcode technology. However, there are some differences in terms of reliability of the technologies. For instance, barcode labels are generally reliable (with some rare exceptions) to read while RFID tags currently are not always reliable and will not work with some products or in certain situations. Therefore to avoid these pitfalls, hospitals will most likely continue to use barcode labeling indefinitely as a fallback when RFID fails, e.g. a barcoded tag using the patient name and ID.
Table of contents :
1 Introduction
1.1 Previous Work
1.2 Problem Statement
1.3 Scope and delimitations
1.4 Thesis Outline
2 Patient Identification Systems
2.1 Patient Safety at the Point of Care
2.2 Overview of Patient Identification Systems
2.2.1 Barcode Identification
2.2.2 Challenges of barcode technology in healthcare
2.2.3 Radio Frequency Identification
2.2.4 Comparison of Barcode and RFID
2.2.5 Challenges of RFID technology in healthcare
2.2.6 Privacy in RFID
2.2.7 Biometric Identification
2.2.8 Smart Card Identification
2.3 Patient identifiers and numbering schemes
2.4 Using handheld devices in hospitals
3 Wireless Networks in Hospitals
3.1 Using wireless networks in hospitals
3.1.1 Applications of wireless networks in hospitals
3.1.2 Issues when using wireless networks in hospitals
3.2 Wireless network security in hospitals
3.2.1 Security concerns with IEEE 802.11 networks
3.2.2 End-to-End Network Security
3.3 Wireless interference in hospitals
3.3.1 Interference factors
3.3.2 Methods to reduce wireless interference
4 The Patient Identification Prototype
4.1 Prototype features and requirements
4.2 Evaluation of design choices
4.2.1 Hardware choices
4.2.2 Software choices
4.3 Prototype construction and development
4.3.1 Software Design
4.3.2 Hardware Construction
5 Testing the Patient Identification Prototype
5.1 Infrastructure and test-bed configuration
5.2 Use case
5.2.1 Actors
5.2.2 Activity diagram
5.2.3 Process flow
5.3 Using the prototype to identify a patient
5.4 Evaluation of the prototype
5.4.1 Observations and effects on patient care
6 Conclusions
6.1 Future Work