Get Complete Project Material File(s) Now! »
The NPY family and their receptors
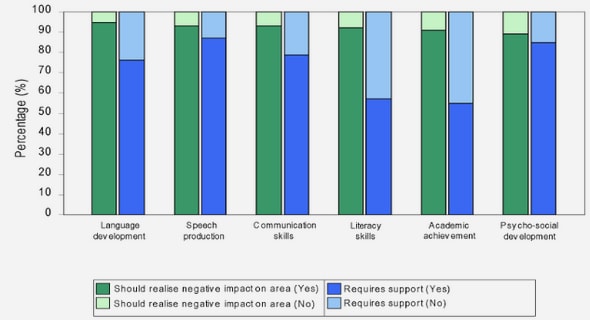
The gut hormone PYY belongs to a family of hormones including two other ones: neuropeptide Y (NPY), and pancreatic polypeptide (PP). They share a same size, 36 amino-acids, and a similar structure with an alpha helix in C-ter and a 3D hairpin structure (Keire 2000) (Figure 15). PYY and NPY have the highest percentage of similarity, with 70% of common residues whereas PP have only 50% common residues with NPY. Moreover, both NPY and PYY can be maturated by cleavage of the two N-terminal residues by the peptidase DPP-IV, modifying their activity (Keire 2002, Mentlein 1993). These peptides are mainly implicated in the control of food intake, but with different effects as NPY is considered as an orexigenic hormone whereas PYY and PP have anorexigenic effects by acting on receptors located at different places. The NPY family is conserved among vertebrates, PP being the less well conserved gene and some functional duplications of this gene have occurred (Ding 1997). Among vertebrates, they share similar tissue expression and functions (Larson 2003, Lundell 2002).
NPY receptors
These hormones are recognized by a specific family of receptors that is also conserved among vertebrates. The family of Y receptor (YR) is composed of 4 receptors in humans, Y1, Y2, Y4 and Y5 and 5 in rodents, y6 being the other one (Larhammar 2004). All of these receptors mainly couple to Gi/o proteins, and therefore signal by decreasing cAMP (Ewald 1988). Thus they can be considered to ave inhibitoyr activities when stimulated. Moreover, it was reported that Y1 and Y4 can have a pertussis independent effect (Misra 2004). PYY and NPY are recognized by Y1, Y2 and Y5. Y1 and Y5 recognize the terminal parts of PYY and NPY whereas Y2 is specific of the loop part of the peptides. Truncation of the two first residues by DPP-IV abrogates their affinity to Y1 and strongly decreases affinity to Y5. Y4 recognize mostly PP and has only weak affinity for PYY (Cabrele 2000, Pedragosa-Badia 2013).
YRs are expressed in the brain, with the highest expression being in the hypothalamus, but also in other tissues including the bones, the adipose tissue, the gut (muscles and epithelium), the vagal nerve, some immune cells, lingual epithelial cells (Ferrier 2002, Lin 2004, Parker 1999).
Intestinal motility, nutrient absorption
Another important role of PYY that is also associated with food intake is control of gut motility and gastric emptying. Indeed, mechanic sensing by vagus nerve is an important message for satiation, and is even the first to develop in infants (Crespi et al, 2014). PYY has been described as one of the hormones inducing the ileal brake that happens in response to entry of nutrients in ileum, where L-cells are present (Maljaars 2008, Lin 2003). Ileal brake consists of a decrease of intestinal motility, inhibition of gastric emptying and inhibition of pancreatic enzymatic and gastric enzyme secretion. Ileal brake is therefore supposed to permit increased absorption in the small intestine. Direct administration of PYY decreases motility and consequently increases gut transit time (Savage 1987). Motility is controlled by two layers of smooth muscles that express Y receptors (Ferrier 2002, Misra 2004).
The contractions of these two layers are also dependent on enterinc neurons. IIeal administration of PYY decreases gastric motility, either in innervated or denervated tissue and decreases gastric contractions (Cuche 2000). Moreover, PYY effect on motility is dependent on its isoform and activation of different receptors. Y2 receptor is only present on circular smooth muscle and enteric neurons whereas Y1 is localized on both smooth muscle layers and on neurons (Misra 2004). Activation of Y2 or Y1 in neurons by PYY 3-36 inhibits motility (Wang 2010, Tough 2011), whereas activation of Y1 by PYY(1-36) directly induces muscle contractility (Ferrier 2000, Ferrier 2002). Thus, PYY has two opposite effects on motility depending on different signaling: a direct pathway which increases muscle contractions and motility and a neuron mediated pathway inhibiting contractions and motility. Its effects are therefore associated with decreased motility by a distal regulation, i.e. in the proximal part of the intestine, corresponding to the gastric and small intestine decreased motility and decreased gastric emptying observed during an ileal brake, and increased motility by local regulation, i.e. mainly in the colon.
Y receptors are expressed on intestinal epithelial cells (Goumain 1998). Thus PYY has direct actions on these cells which include decreased histamine secretion by ECL cells, and therefore decreases gastric acid secretion (Yang 2002, Cloarec 1989, Bado 1993), and decreased pancreatic enzymes secretion (Adrian 1985). In the colon, PYY has an important role in controlling water reabsorption and electrolyte intake (Quin 1995, Nakanishi 1996, Cox 2002) by decreasing basal short circuit currents created by chlorure secretion. In the colon and small intestine crypt, Na+ and Cl- ions are absorbed in an electroneutral way, depending on exchange with a proton and a bircabonate, but Cl- is also secreted, depending on cAMP activation (Sandle 1998). Activation of Y2 receptor has an antisecretory activity of electrolytes (Cox 2008), which is thus associated with increased absorption of electrolytes. Regulation of electrolyte secretion is a way to control water and nutrient absorption maintaining osmotic gradient. PYY participates therefore in the regulation of water absorption by colon (Sandle 1998), and PYY 3-36 has anti diarrhea effects (Moriya 2010) through activation on Y2 receptor.
PYY has also been implicated in lipid metabolism in intestinal epithelial cells (Grenier 2012) as basolateral administration of PYY on polarized Caco2 cells decreases formation of chylomicrons and regulates expression of several enzymes implicated in lipid homeostasis.
Effect of fiber rich diets and SCFA administration on PYY plasma levels
Fiber rich diets increase SCFAs concentration in the colon. Use of different fiber sources in humans or in rodent models could show their influence on PYY plasma concentration (Arora 2012, Cani 2009, Delzenne 2005, Parnell 2012, Reimer 2012, Zhou 2008). Long term effects could be associated with modification of microbiota (De Filippo 2010, Neyrinck 2012, Wu 2011), including increased proportion of Prevotella spp., increased Firmicutes and decreased Bacteroides. Effects of fibers on PYY is dependent on their degradation by microbiota as in germ free animals PYY plasma levels were not affected whereas colonization with minimal microbiota enabling fermentation induced a PYY rise (Samuel 2008). However, in this study, only one fiber rich diet was tested and other effects due to presence of minimal microbiota per itself were not assessed.
Change of diet and increased colonic SCFAs concentration induced long term effects, including increased plasma levels of PYY and higher PYY content in colonic tissues, but the precise mechanisms implicated in these responses could not be precisely determined. Higher gene expression in tissue can be a consequence of either an up regulation of gene expression per cell or increased number of enteroendocrine cells producing the hormone. As L-cells are sparse in the epithelium, mRNA content per cell could not be assessed except in rodent models expressing specific markers for L-cells or in cellular models. SCFAs were shown to increase the number of L-cells in organoid models (Petersen 2014), but with differences between human organoids and mouse organoids concerning modulation of transcription factor expression. Similarly, diet supplemented with non-digestible carbohydrates increased number of L-cells in rats (Cani 2007, Kaji 2010) and mice (Everard 2011). Mice lacking FFAR2 or FFAR3 have been used to test the importance of these receptors in the response to SCFAs. In axenic mice, effect of colonization enabling fiber fermentation was reduced in ffar3-/- mice compared to ffar3+/+ littermates, indicating that ffar3 may be implied in the response of L-cells to SCFAs. Interestingly, in this study, SCFAs concentration was more important in the feces of ffar3-/- mice compared to ffar3+/+ mice, indicating that ffar2 may also be implicated in regulation of SCFAs absorption (Samuel 2008).
Expression of PYY has not been tested in cellular models, except promoter activity of rat PYY in human epithelial kidney cells (HEK) in which PYY expression was increased by SCFAs at different concentrations. However, the conclusions of this study are limited by the fact that HEK cells do not express receptors similarly to EEC and the use of orthologous promoter (Zhou 2008). As Pyy gene structure is very different between humans and rodents, conclusions concerning regulation of Pyy expression from rodent may not be relevant for humans. Expression of proglucagon, the GLP-1 and GLP-2 prohormone is increased in rodent cell line STC-1 models (Zhou 2008) but decreased in human cell line NCI-h716 (Cao 2003) by butyrate. As both models are cell lines, differences of SCFA effect may be cell line dependent or species dependent due to different promoters (Nian 1999). Enteroendocrine cells being secreting cells, most studies were interested in regulation of secretion in these cells.
Regulation of secretion by SCFAs
Direct administration of SCFAs in human or rat colon rapidly increased PYY plasma levels (Cherbut 1998, Chambers 2014, Freelend 2010), indicating that SCFAs can directly induce secretion. Interestingly, rectal administration of acetate in humans did had a much stronger effect than intravenous administration, suggesting that acetate is sensed in the lumen of the colon rather than from the circulation (Freelend 2010). Moreover, in vitro, administration of propionate on human colonic crypts isolated from biopsies increased PYY secretion during a 2h incubation test. However, only non-physiologic concentration of propionate could induce this effect as only concentrations higher than 100mM had an effect (Chambers 2014). Similar results were published in the same time using murine colonic crypts, but secretion was stimulated by much lower propionate concentrations, as low as 1mM (Psichas 2015). In STC-1, propionate or butyrate had no effect on secretion of PYY, but only submillimolar doses where tested (100 M) (Hand 2012). Effect of SCFAs on secretion in L-cells has been mainly studied by assessing the secretion of GLP-1. As PYY is co-secreted with GLP-1, it can be assumed that GLP-1 secretion is associated with PYY secretion (Habib 2013).
An elegant strategy to sort L-cell population for further studies is to express specifically a fluorescent protein with a specific L-cell promoter such as the proglucagon promoter (Reimann 2008). Incubation of these cells with single SCFA at millimolar dose increased GLP-1 secretion. L-cells isolated from ffar2-/- or ffar3 -/- mice had a decreased secretory response to acetate and propionate compared to L-cells from WT mice (Tolhurst 2012). In another study, mice lacking ffar2 had similar levels of circulating PYY in the portal vein, but direct administration of propionate in the colon decreased PYY induced secretion. Moreover, basal secretion by colonic crypt from ffar2-/- mice during two hours was similar to secretion by colonic crypt from WT mice, but secretory response to propionate was decreased in k.o. mice (Psichas 2015). These studies therefore indicated that both ffar2 and ffar3 may be implicated in the responses to SCFAs in mice. However, ffar2-/- mice had lower expression of ffar3 compared to ffar2+/+ mice (Tolhurst 2012), indicating potential regulation of the expression of these two receptors by each other. Thus, even if effect of SCFA at millimolar dose increased secretion in L-cells, precise pathways need to be determined, as well as vailidity of this effect in humans as only higher doses of propionate could induce a secretory response. Moreover, a third receptor can be implicated in the response to SCFAs in the intestine, GPR109a, and has been hypothesized as being implicated in the response to SCFAs in L-cells (Thangaraju 2009, Kaji 2014).
SCFAs regulate PYY plasma levels through different pathways, which may be different between species due to different receptors affinity, signaling pathways and promoter regulation. One of our objective in this project was to decipher the precise mechanisms involved in SCFAs effects on L-cells in humans. We took advantage of described cell lines modelling enteroendocrine cells to monitor precisely the effects of SCFAs on PYY production and secretion by these cells, and could use cellular tools to demonstrate implication of different mechanisms implicated in the response of L-cells to SCFAs.
Role and structure of TLRs in the recognition of MAMPs
A well described communication between microbes and host cells is through recognition of Microbial Associated Molecular Pattern by the Toll-Like Receptors (TLRs). This system was first identified as an important mechanism for innate immunity. TLRs allow recognition of potential pathogens in immune cells and non-immune cells and induce a pro-inflammatory response by activating NF- B pathway and secreting cytokines. Other families of receptors implicated in the innate response to pathogens have been identified and form a super family of patter recognition receptors including additionally to TLRs Retinoic acid-inducible gene like receptors (RLR) and Nucleotide-binding oligomerization domain (NOD) and NOD-like receptors (NLR) (Medzhitov 2007, Akira 2006). Whereas RLRs and NLRs are intracellular receptors sensing compounds that cross the plasma membrane, TLRs are membrane receptors ever localized on the plasma membrane sensing extracellular content or on endosome membrane sensing endocytic content.
TLRs family is composed of ten different functional receptors, TLR1 to TLR10, in humans and 11 in mice, with high similarity between most of them. However, mouse TLR8 is not functional, have no TLR10. TLR11, TLR12 and TLR13 are expressed in mice but not present in humans. Heterologous receptors recognize similar patterns, enabling functional characterization of TLRs in mice. However, function of TLR10 which was much recently described is less known, but seems to have inhibitory effect on TLR2 dependent inflammatory response (Oosting 2014). Rapidly, TLRs can recognize mainly two families of molecules: TLR1, 2, 4, 5 and 6 recognize membrane associated molecules including lipoproteins, peptidoglycans, lipopolysaccharide and flagellin whereas TLR3, 7, 8 and 9 recognize bacterial and viral DNA or RNA patterns. Recognition of these molecules is associated with localization of receptors: TLR1, 2, 4, 5 and 6 are plasma membrane receptors whereas TLR3, 7, 8 and 9 are mainly present in endosomes. TLR1 and TLR6 require to be associated with TLR2 in heterodimers to recognize respectively triacyl lipoproteins and diacyl proteins (Kumar 2009, Kawai 2007) (Figure 19).
Activation of TLRs induces well characterized signaling cascades leading to activation and translocation into the nucleus of transcription factors NF- B and AP-1. Rapidly, two main pathways have been described: recruitment and activation of adaptors TIRAP and MyD88 or recruitment of TRIF. Both of them induce NF- B activation. All TLRs except TLR3 can activate MyD88 pathway whereas only TLR3 and TLR4 can activate TRIF pathway. Other non-canonical pathways have been described and regulate different responses. (Kawai 2007, Kawasaki 2014). NF- B is a dimer composed of two subunits of a family of five subunits, p65, RelB, C-Rel, P50 (which precursor is p105) and P52 (which precursor is p100). The main form activated after TLR activation is p50-p65 heterodimer; heterodimer p52-RelB and homodimer p50-p50 are mostly implicated in non-canonical NF- B activation. NF- B dimer is sequestered in the cytoplasm by a family of inhibitors, I B, which is inactivated and further degraded when phosphorylated by a complex IKK in response to TLR activation. In the nucleus, NF- B promotes gene expression by binding to consensus binding site (Cogswell 1994, Udalova 2002, Martone 2003). Genes regulated by NF- B are mainly genes implicated in inflammatory response, including different cytokines like Il-1, Il-8, interferon- or TNF- . Other responses associated with NF- B activation are mainly stress response, regulation of adhesion or apoptosis as NF- B binding domain site is present in the promoter of many genes (Pahl 1999, Gilmore 2006) (Figure 20).
TLRs in epithelial cells and enteroendocrine cells
Intestinal epithelial cells are continuously in direct contact with microbes present in the lumen and form an active barrier between commensal bacteria and the host. Epithelium prevents internalization of microbes, but also modulate immune response to shape microbiota and participates in the regulation of immune cells by secreting different cytokines (Stadnyk 1994). However, their response must be limited to avoid induction of inflammation whereas they are exposed to a high number of microbes. Moreover, presence in the epithelium of dentritic cells and T cells, that express TLRs at high levels, participate in the sensing of microbial communities and response. Intestinal epithelial cells have been demonstrated to express all TLRs except TLR10 (Abreu 2010, Graves 2014). Localization of TLRs is important as depending on localization on apical membrane or basolateral membrane, they are exposed very different quantities of MAMPs.
Table of contents :
Introduction
The gastrointestinal tract
The digestive system, vital functions for the host
Components of the digestive system
Structuration of the gut wall
Gut microbiota
Intestinal epithelium
Enterocytes, Transport and cell junctions
Goblet cells and Mucus
Paneth cells
Tuft cells
Enteroendocrine cells
Intestinal stem cells
Cell differentiation
Enteroendocrine cells differentiation
Enteroendocrine cells
Role of enteroendocrine cells
Gastric hormones
Enzymatic secretion regulation
Gut motility regulation
Incretin hormone
Food intake control
Production and secretion of hormones
Regulation of hormonal production
Regulation of secretion in enteroendocrine cells
L-cells
Peptide YY
The NPY family and their receptors
NPY receptors
PP, NPY and PYY
Functions of PYY
Regulation of food intake by PYY
Intestinal motility, nutrient absorption
Metabolism
Bacterial products implicated in cross talk with EEC
Functional metagenomics to search for new bacterial genes regulating PYY expression and secretion
Short chain fatty acids
SCFAs production in the colon
Bacteria implicated in SCFAs produciton
SCFAs transport
SCFAs, Inhibitors of HDAC
SCFAs Receptors.
Effect of fiber rich diets and SCFA administration on PYY plasma levels
Regulation of secretion by SCFAs
MAMPs and TLRs
Role and structure of TLRs in the recognition of MAMPs
TLRs in epithelial cells and enteroendocrine cells
Model Development
Development of a reporter system for Pyy gene expression
Classical reporter systems
DNA repair to induce mutations or integrate a specific sequence
DNA double strand break
Strategy for a fluorescent reporter gene integrated in Pyy coding gene
Development of reporter systems for secretion
Calcium sensors
Live imaging for calcium imaging
Image analysis
Material and methods:
Cell coating, cell sorting and transfection
Plasmid construction
Results
Short Chain Fatty Acids differently regulate Peptide YY expression and secretion in human
enteroendocrine L-cells
Microbial sensing by TLRs in L-cells is increased by butyrate and modulates Pyy expression
Discussion
In vitro cellular models to study PYY release by L-cells
Modulation of PYY plasma levels
Importance of gene expression regulation
Differences between human and rodent Pyy encoding gene
PYY secretion in humans and rodents
Human cell lines modeling L-cells
Limitation of cell lines
Organoids, a future in in vitro studies?
Importance of microbial sensing by L-cells
Sensing of microbial products
Regulation of PYY expression by SCFAs
Mechanisms implicated in the response to SCFAs in the modulation of gene expression
Regulation of Pyy by microbial products through activation of receptors
Concentration of SCFAs sensed by L-cells
Regulation of PYY production by SCFAs
Regulation of secretion by SCFAs
SCFAs modulate sensing in L-cells
SCFAs and metabolism in L-cells
Beneficial effects of regulation of PYY production and secretion
PYY in germ-free animals
Genetics of PYY and obesity
Effect of SCFAs to modulate secretion for its anorexigenic effects
Obesity, microbiota, SCFAs and TLRs
Microbiota and PYY interrelations
Bibliography