Get Complete Project Material File(s) Now! »
Clinical Features of Behçet’s Disease
A systemic disease, BD may affect almost all vascularized body systems and is characterized by episodes of relapses and remissions leading to sequelae.1,11,12,185 Although several clinical manifestations are associated with BD, the triple-system complex of oral and genital aphthae and uveitis first described by Behçet in 1937 generally illustrates disease pattern. Clinical manifestations in children (<16 years) resemble those of adults.20,21 Children exhibit more frequent perianal aphthosis and arthralgia, less frequent genital ulcers and vascular involvement, and a more severe course of uveitis.1,186 Over the past few years, modern treatment strategies, involving immunosuppressant therapy and the use of aggressive approaches have led to improvements in the prognosis of severe forms of BD.4,187 Prognosis for the disease is usually reserved, especially when ocular, cardiovascular, neurological, and / or gastrointestinal manifestations appear.5,185,188
Oral Ulcers
Recurrent oral ulcers represent the earliest disease manifestation in 47-86% of patients.188 It may take years for the other symptoms to appear afterwards, and oral ulcers are observed in all patients during their clinical course. Lesions resemble common oral aphthous ulcers, but are more painful and wider. They have disciform appearance with round and sharp erythematous border, covered with a grayish-white pseudomembrane or a central yellowish fibrinous base and grow rapidly from a flat ulcer to a deep sore.1 They may occur as single ulcers or in crops and heal with little scarring.1,2 Oral ulcers most commonly affect the gingival and buccal mucosa, tongue and lips, yet may also appear in the soft and hard palates, pharynx and tonsils.1 In certain cases, oral ulcers derive from buccal trauma. Minor ulcers (<1 cm in diameter) heal without scarring in 4-14 days whereas major ulcers (>1 cm in diameter) are more painful and heal with scarring in 2-6 weeks. Herpetiform ulcers occur in recurrent crops of small sores that are 0.2-0.3 cm in diameter, are painful and may coalesce. Treatment is usually symptomatic and prognosis of oral ulcerations is favorable.2,188
Genital Ulcers
Genital ulcers develop in 57-93% of patients.5 They are painful and morphologically resemble oral ulcers, but are larger, deeper, have more irregular margins and heal with white or pigmented scars.188 Male genital lesions most commonly involve the scrotum and usually leave a scar that will help with the diagnosis retrospectively. They may also affect the epididymis; penile lesions are less frequent.1 In females, vulvar, vaginal and cervical lesions are especially common.2 Rarely, deep vaginal lesions may perforate the bladder resulting in fistulae.5,188 Both males and females may develop perineal, perianal and groin lesions.188 In cases of fistulae and internal lesions, prognosis is unfavorable when the infectious risk is inadequately evaluated.1,2
Ocular Manifestations
Ocular disease, involving the retina and the uvea, occurs in 30-70% of BD patients and is associated with high morbidity.4 It is the primary cause of blindness in approximately 25% of patients despite aggressive corticosteroid treatment.4 Ocular symptoms occur more frequently in males and are associated with disease severity, even though prognosis is improving with the use of aggressive immunosuppressant therapy.1,2 They usually occur two-three years after the onset of oral or genital ulcerations but remain the first disease manifestation in 10-20% of patients.1 Typically, ocular disease is a chronic relapsing bilateral non-granulomatous uveitis that may involve the anterior segment, the posterior segment, or both (panuveitis).185,186 The latter is associated with a worse prognosis and is more common among males.1 Ocular disease is characterized by the formation of hypopyon: a visible layer of pus in the anterior chamber observed in approximately one-third of patients.2 Episodes of anterior uveitis subside spontaneously yet repeated attacks result in irreversible structural deformities.7,186 Ocular inflammation also includes iridocyclitis, keratitis, episcleritis, scleritis, vitritis, vitreous hemorrhage, retinal vasculitis, retinal vein occlusion, retinal neovascularization, and optic neuritis.4
Symptoms include blurred vision, photophobia, lacrimation, floaters, hyperemia and periorbital or global pain.1,2 Recurrent inflammatory attacks are associated with secondary complications such as posterior and peripheral anterior synechia, iris atrophy, cataracts resulting from inflammation or treatment, secondary glaucoma (occasionally neovascular), atrophic retina, optic atrophy, macular edema, macular degeneration, retinal veins occlusion, sheathed vessels, chorioretinal scars and proliferative vitreoretinopathy and phthisis bulbi.1,4 Prognosis is correlated with frequency, severity of ocular inflammation, and extent of lesions, and remains in many cases unfavorable.4
Cutaneous Manifestations
Skin involvement affects 38-99% of BD patients.1,11 Cutaneous manifestations commonly include papulopustular (28-96%) and acne-like lesions.5,20 Wounds exhibit a wide distribution affecting the face, limbs, trunk and buttocks.1 Skin lesions are characterized by thrombosis and vasculitis.11 Early lesions exhibit leukocytoclastic vasculitis or neutrophilic vascular reactions whereas mature lesions are characterized by lymphocytic vasculitis.5
Erythema nodosum lesions occur in 15-78% of patients, mainly in females and in the lower limbs.1,2 These lesions are painful, may form ulceration and usually heal leaving residual pigmentation. Cutaneous ulcers are rare and only affect 3% of BD patients.1 They resemble aphthous ulcers, are recurrent, and typically heal with scarring. They appear in the neck, breast, axillae, inguinal region, legs and interdigital skin of the feet.188 Prognosis for most cutaneous lesions in BD is usually favorable.1
Cardiovascular Manifestations
Behçet’s disease may affect blood vessels of different sizes and types, including arteries and veins as well as the heart organ.189 Cardiovascular features were reported to affect 7-49% of patients, more frequently males.1,190 They occur approximately 3-16 years after the onset of BD.13
Vascular BD commonly affects veins causing recurrent superficial thrombophlebitis and deep venous thrombosis in 30-40% of patients.7,191,192 Thromboses of the superior and inferior vena cava (0.2-9% of patients), dural sinuses and supra-hepatic veins (2-3.2% of patients), and pulmonary arterial aneurysms (1% of patients) may also occur and are associated with poor prognoses.1,189,192 Occlusion and aneurysms of major arteries commonly lead to bleeding, infarction, organ failure and restricted movements of arms and legs.2 Rupture of aneurysms may be fatal. At the level of lungs, thrombosis, aneurysm, and arteriobronchial fistula cause recurrent episodes of dyspnea, cough, chest pain and hemoptysis.2
Cardiac involvement includes pericarditis, myocarditis, endocarditis, mitral valve prolapse, valve lesions, intracardiac thrombosis, endomyocardial fibrosis, myocardiopathy, and coronary artery lesions, and is the result of systemic vascular involvement.29,190,193 The prognosis in these cases is unfavorable with frequent recurrences.1,193 The highest direct mortality rate in cardiovascular involvement was attributed to large vessel vasculitis as a result of sudden death by aneurysm rupture or thrombosis (9.8% of patients in one study in Turkey).21,190,194
Neurological Manifestations
Neurological involvement in BD (neuro-BD) occurs in 5-10% of patients and is more frequent in males.7,8,37 It usually occurs around five years after the onset of the disease and is associated with long-term morbidity and mortality.1,195 Neurological disease affects the CNS more frequently than the peripheral nervous system.196,197 Headache syndromes represent the most common neurological symptom and occur in 70% of patients.7,198 Neuro-BD may be parenchymal (80% of patients), non-parenchymal, or mixed brain disease.1,7 Parenchymal brain disease affects the brainstem and / or basal ganglia and is correlated with a particularly poor prognosis.7,199 Non-parenchymal brain disease is characterized by dural sinus thrombosis, arterial vasculitis, and aseptic meningitis, and comprises the most devastating symptom category of BD.7,37
Most parenchymal neuro-BD cases present as meningoencephalitis (75%) that exhibit subacute onset and are associated with exacerbation of systemic manifestations.195,196 Flare-ups peak within a few days and may last for periods of weeks. Brainstem involvement, including ophtalmoparesis, cranial neuropathy, and cerebellar or pyramidal dysfunction, has additionally been reported.1,7,197,200 Cerebral or spinal cord involvement was observed in association with subcortical dementia, accompanied by ataxia.195,199 Cerebral hemispheric involvement, including encephalopathy, hemiparesis, hemisensory loss, seizures and dysphasia, and mental changes, including cognitive dysfunction and psychosis, were observed as well.7,8,201 Spinal cord involvement, manifested by pyramidal signs in the limbs, sensory level perturbance and sphincter dysfunction, has also been reported.7,201,198 Other less common clinical symptoms involving the CNS were reported as well such as: stroke, epilepsy, brain tumor-like neuro-BD, movement disorders, acute meningeal syndrome, optic neuropathy, spinal cord involvement and asymptomatic and subclinical neurological involvement.195,200,202
Non-parenchymal neuro-BD, also referred to as vasculo-BD or angio-BD, involves the main vascular structures of the CNS.197 Clinical syndromes include vascular disorders, intracranial hypertension, and intracranial aneurysms.203 More rarely, mixed parenchymal and non-parenchymal disease were reported with limited collected data.203
Classically, meningitis or meningoencephalitis, neurological deficits including motor disturbances, and brainstem symptoms and psychiatric symptoms including personality changes develop in patients with neuro-BD.2,7 These symptoms are associated with disease exacerbations and gradually cause irreversible disability.2 At late stages, dementia develops in approximately one-third of patients. As such, psychiatric or cognitive symptoms may represent the first manifestation of neuro-BD.2,204 Cognitive impairment in neuro-BD patients includes poor memory, attention and motivation, in addition to personality changes.204 Psychosomatic symptoms, including anxiety and depression, are the most common psychiatric symptoms in BD and physicians must remain particularly attentive to other causes of psychiatric morbidity; however, these manifestations are rarely a result of direct CNS involvement. Prognosis for neuro-BD, in all its forms, is unfavorable.5,7,198
Articular Manifestations
Articular involvement occurs in 45-60% of patients and includes either monoarthritis or polyarthritis.205 Articular disease includes arthralgia, arthritis and synovitis.205 Non-erosive, non-deforming oligoarthralgia commonly involving the knees, ankles, elbows, and wrists is the most frequent manifestation.1,2 Neutrophilic and mononuclear cell infiltrates in the synovium and small-vessel lesions with thrombosis typically characterize articular disease.2 Destructive changes rarely occur in patients with articular involvement.206 As anti-inflammatory treatment is generally effective, prognosis is generally favorable.207
Gastrointestinal Manifestations
Gastrointestinal involvement occurs in 3-26% of patients and varies among different populations.9,208 It is much more frequent in Japan than in the Middle East and the Mediterranean region.1,19,11 Mucosal inflammation and ulceration occur throughout the gastrointestinal tract and are generally located in the ileocaecal region.9,208 The esophagus, ascending colon, and transverse colon are less frequently involved.2 Clinical symptoms include anorexia, vomiting, dyspepsia, diarrhea, melena, abdominal pain and, less frequently, perforation requiring surgical intervention.207,209 Prognosis is unfavorable as gastrointestinal involvement is typically acute and chronic.
Diagnosis of Behçet’s Disease
A Behçet’s disease diagnosis is typically confirmed by elimination of other disease scenarios, even when a triple-symptom complex is evident. As there exists no targeted diagnostic test for BD, diagnosis of clinical symptoms is challenging, especially when symptoms are non-concomitant. Investigating the clinical history of patients helps exclude other conditions during diagnosis of BD. These conditions include Reiter’s syndrome, sarcoidosis, Stevens-Johnson syndrome, familial Mediterranean fever, multiple sclerosis, systemic lupus erythematosus, mixed connective tissue diseases, celiac disease, inflammatory bowel disease (Crohn’s disease and ulcerative colitis), Herpes Simplex virus infection, syphilis, Sweet’s syndrome, Vogt-Koyanagi-Harada syndrome, bullous skin disorders, erythema multiforme, recurrent aphthous stomatitis, seronegative arthropathies, and Easle’s disease.1 For instance, differentiation between the gastrointestinal involvement in BD and inflammatory bowel disease is often difficult due to the similarity in the extraintestinal symptoms (oral ulceration, erythema nodosum, uveitis and arthritis). In addition, intestinal ulceration in BD patients is indistinguishable from that in patients with ulcerative colitis. Likewise, neurological involvement in BD patients may be misdiagnosed as multiple sclerosis. Distinguishing features, such as granuloma formation in patients with Crohn’s disease and negative pathergy test in patients with inflammatory bowel disease, may help with the differential diagnosis. HLA typing and measurement of serum IgD levels, which are known to be elevated in patients with active BD, may also be helpful.2
In the absence of a universally accepted diagnostic test, detection of BD has centered on the identification of a number of the typical clinical features associated with the disease. Over the years, five major independent sets of criteria were proposed for the diagnosis of BD, each characterized by its own clinical features and number and nature of criteria that should be met in order for the diagnosis to be positive.3,33 Notably, all the different sets of diagnostic criteria shared the three major symptoms initially described by Behçet as a separate clinical entity (oral ulceration, genital ulceration, and eye lesions).1
At present, there are no or few findings specific for BD.1 Elevated levels of inflammatory markers may be associated with the disease. These include C-reactive protein, erythrocyte sedimentation rate, peripheral leukocyte and platelet counts and serum cytokines (TNFα, IFNγ, IL-1β, IL-6 and IL-8). Moderate anemia of chronic disease may also be present; however, autoantibodies, such as antinuclear antibodies and rheumatoid factor, are usually absent.1
According to Mason and Barnes (1969), diagnosis of BD was positive when three major criteria or two major and two minor criteria were present.210 Major criteria included oral ulceration, genital ulceration, eye lesions (uveitis, corneal ulceration, retrobulbar neuritis) and skin lesions (pustules, ulceration, erythema nodosum, erythema multiforme). Minor criteria included gastrointestinal lesions, thrombophlebitis, cardiovascular lesions, arthritis, CNS lesions, and family history.
Another set of diagnostic criteria was proposed by BD Research Committee of Japan in 1972, and was subjected to revision in 1987 and 2003.211,212 These diagnostic criteria classified the disease as complete, incomplete and suspected. Complete disease was considered when four major criteria were present, incomplete disease when three major criteria, two major and two minor criteria or typical recurrent ocular symptom along with one major or two minor criteria were present, and suspected disease when one or two major criteria were present. Major criteria comprised recurrent aphthous ulceration of the oral mucous membrane, skin lesions (subcutaneous thrombophlebitis, folliculitis, acne-like lesions, cutaneous hypersensitivity), eye lesions (iridocyclitis, chorioretinitis, retino-uveitis, definite history of chorioretinitis or retino-uveitis) and genital ulceration. Minor criteria involved arthritis without deformity or ankylosis, gastrointestinal lesions characterized by ileocaecal ulcers, epididymitis, vascular lesions, and CNS symptoms.
In 1974, O’Duffy considered positive diagnosis of BD when oral or genital ulceration along with two other criteria and vasculitis in tissue biopsies were present.213 Major criteria included oral ulceration, genital ulceration, uveitis and dermal vasculitis (erythema nodosum). Minor criteria included arthritis, CNS involvement, colitis, phlebitis and large vessel arteritis.
Subsequent diagnostic criteria included a positive pathergy test. Zhang (1980) considered complete disease when three major or two major and two minor criteria were present and incomplete disease when patients exhibited two major, or one major and two minor criteria.214 Major criteria included oral ulceration, genital ulceration and uveitis. Minor criteria included skin (erythema nodosum, erythema multiforme, pathergy), arthritis, vasculitis (thrombophlebitis, arteritis, aneurysm), pulmonary (hemoptysis, lung infiltration, interstitial fibrosis), gastrointestinal lesions (ulceration, bleeding, perforation), renal (renal damage, ulceration of bladder, hematuria, epididymitis) and neurological features. In 1986, Dilsen et al. also proposed a set of diagnostic criteria that included a pathergy test.215
More recently, an International Study Group (ISG) for BD, which was founded during the Fourth International Conference on BD (1985) in London, compared the performance of the previously defined sets of benchmarks and established a new internationally approved set of diagnostic criteria for BD. The ISG included proponents of four of the five previously described sets of diagnostic criteria in an attempt to agree on one set to be quoted in all future work, and thus enable comparison between studies and promote collaborative research. These criteria, published in 1990 (and updated in 2013) provided simpler means for diagnosis of BD, and unlike the previously defined sets of criteria, excluded rare and subjective features and showed more specificity with little or no loss of sensitivity.2,16 The new set of diagnostic criteria proposed by the ISG imposed the presence of recurrent oral ulceration, in addition to any two of recurrent genital ulceration, eye lesions, skin lesions or positive pathergy test. Recurrent oral ulceration included minor aphthous, major aphthous or herpetiform ulceration observed by a physician or patient and recurring at least three times in a 12-month period. Recurrent genital ulceration included aphthous ulceration or scarring observed by physician or patient. Eye lesions included anterior uveitis, posterior uveitis or cells in vitreous on slit lamp examination, or retinal vasculitis, and observed by an ophthalmologist. Skin lesions included erythema nodosum observed by the physician or patient, pseudofolliculitis or papulopustular lesions, or acneiform nodules observed by a physician in post-adolescent patients not receiving corticosteroid therapy. Finally, positive pathergy test was to be read by a physician at 24-48 hours.
Likewise, there is no diagnostic test for neuro-BD, and thus diagnosis of neurological involvement in BD is based on clinical aspects.198 However, unlike BD, no criteria were established for the diagnosis of neuro-BD. In such cases, analysis of blood work, and CSF and MRI examination provide nonspecific tools for the diagnosis of neurological involvement.7,198
Measurement of disease activity is essential for the assessment of disease progression and for proper clinical management. Several forms were proposed for the assessment of the clinical activity of BD.1 These include the Iranian BD Dynamic Activity Measure, the European BD Current Activity Form, and the standard proposed by the BD Research Committee of Japan.
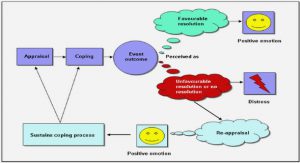
In 2004, Lawton et al. conducted a study in an attempt to define a set of clinical features that can be used as a standard index for measurement of BD activity, and thus provide international means for monitoring disease progression, clinical management, and evaluating the efficacy of therapeutic interventions.15 Five countries participated in this study, namely China, Korea, Iraq, Turkey and UK. Between 1995 and 2002, 542 BD Current Activity Forms were completed. Using the Rasch method, the study analyzed fourteen items, previously defined to form an index of disease activity. These items included the presence or absence of arthralgia, arthritis, diarrhea, erythema nodosum, eye inflammation, genital ulcers, headaches, mouth ulcers, nausea / vomiting, new CNS involvement, new major vessel inflammation and pustules over the last four weeks prior to the clinic visit, in addition to a Likert scale. The latter is represented by « smiley » faces ranging from very bad to very good and describes how the patient or the clinician felt the disease activity had been over the last four weeks. It was inferred that the BD Current Activity Form provided a convenient tool that may be used to develop an overall score for disease activity, that can serve as an index in clinical trials involving therapeutic interventions.14,15
Treatment of Behçet’s Disease
As no curative solution is currently available, treatment of BD attempts to relieve symptoms, resolve inflammation, limit tissue damage, reduce recurrence frequency and severity, and avoid life-threatening complications.1 Choice of treatment depends on the combinations of clinical symptoms and the severity of organ involvement, with priority given to treatment of ocular, gastrointestinal, CNS, and cardiovascular manifestations.17
EULAR Guidelines
Mendes et al. (2009) summarized the recommendations of the European League Against Rheumatism (EULAR) for the management of BD.1 The recommendations combined current evidence from clinical trials and were developed by a multidisciplinary expert committee. The committee included specialists from six European countries plus Tunisia and Korea and consisted of nine rheumatologists, three ophthalmologists, one internist, one dermatologist, and one neurologist, in addition to a patient representative.
Nine recommendations were developed for the treatment of BD in its different aspects (eye involvement, refractory eye involvement, major vessel disease, anticoagulation, gastrointestinal involvement, joint involvement, neurological involvement, cyclosporine A neurotoxicity, and mucocutaneous involvement). The recommendations target all doctors and surgeons who are involved in the treatment of BD and are summarized in Table 1 below.
Table of contents :
1.! Introduction
2.! NOD Model of Autoimmunity
3.! Autoinflammation in Behçet’s Disease
4.! Systemic Vasculitides
5.! Behçet’s Disease
6.! Clinical Features of Behçet’s Disease
6.1.! Oral Ulcers
6.2.! Genital Ulcers
6.3.! Ocular Manifestations
6.4.! Cutaneous Manifestations
6.5.! Cardiovascular Manifestations
6.6.! Neurological Manifestations
6.7.! Articular Manifestations
6.8.! Gastrointestinal Manifestations
7.! Diagnosis of Behçet’s Disease
8.! Treatment of Behçet’s Disease
8.1! EULAR Guidelines
8.2.! Therapies
9.! Prognosis of Behçet’s Disease
10.! Study Cohort
10.1.! Methodology
10.2.! Results
10.3.! Discussion
11.! Conclusion
Acknowledgement
References