Get Complete Project Material File(s) Now! »
HCV viral particle components in viral entry
Though human hepatocytes are the major targets of HCV, increasing evidence have shown the existence of HCV in extrahepatic organs, such as peripheral blood mononucleated cells (PBMCs) and lymphoid cells including T lymphocytes, B lymphocytes and B-cell lymphoma cells (Laskus et al., 1998; Sung et al., 2003; Bare et al., 2005; Kondo et al. 2007; Murakami et al., 2008; Kondo et al., 2011; Sarhan et al., 2012). The lymphotropism and direct interaction of HCV with these cells could explain the carcinogenesis of the lymphoid cells and the disorders of host immune response in HCV persistent infection (De Vita et al., 1995; Weng & Levy, 2003; Machida et al., 2005; Rosa et al., 2005). HCV RNA-positive PBMCs such as monocytes and dendritic cells, as well as lymphoid cells were also described as potential reservoirs that may contribute to the recurrence of HCV infection and clinically difficult-to-treat extrahepatic diseases (Barth et al., 2005; Coquillard & Patterson, 2009; Pham et al., 2008; Pham et al., 2010). Moreover, recent reports have shown that HCV can establish infection in neuroepithelioma-derived cell lines and endothelial cells of the blood-brain barrier (Fletcher et al.2010; Fletcher et al., 2012), which could offer a clue to the central nervous system (CNS) abnormalities in chronic HCV-infected patients (Weissenborn et al., 2009). As HCV is mainly hepatotropic, substantial in vitro studies on HCV infection were carried out in hepatic-derived cells such as Huh7 cells and HepG2 cells. HCV initiates its infection by entry into host cells. There exists at least two routes: cell-free infection and cell-cell transmission (Valli et al., 2006) (Fig.17). The infection by cell-free HCV particles can be blocked by anti-E2 neutralizing antibodies or in agarose-containing culture, whereas direct transmission of virus between cells does not involve the release of viral particles into the extracellular space, and is relatively nAbs-resistant (Witteveldt et al., 2009; Calland et al., 2012). Notably, HCV cell-to-cell transmission requires cell-cell contacts and the assembly of infectious viral particles in the donor cells, since no cell-cell transmission was observed when the donor cells were electroporated with viral RNA lacking the envelope proteins E1E2-encoding regions (Timpe et al., 2008; Witteveldt et al., 2009). These findings provided potential mechanisms that can partly explain the ineffectiveness of serum anti-HCV antibodies in controlling HCV chronic infection, in addition to the conventional genetic escape mechanism such as the “quasispecies” nature of HCV in the bloodstream and the high rate of amino acid subsitutions in the neutralization epitopes located in HCV envelope glycoproteins (von Hahn et al., 2007). Of note, cell-free transmission route are most likely responsible for the spread of HCV between hosts, and HCV reinfection in liver allograft patients after transplantation, while HCV cell-cell transmission probably is the dominant route of virus propagation in chronically infected individuals. The cell-to-cell spread is more efficient than cell-free infection, which has been found in many other viruses including Vesicular Stomatitis Virus (VSV), Cytomegalovirus (CMV), Vaccinia Virus (VV), Human T-lymphotropic Virus (HTLV-I) and human immunodeficiency virus HIV (Sweet et al., 1999; Cole & Grose, 2003; Igakura et al., 2003; Simth & Law, 2004; Dale et al., 2011). To demonstrate the transmission routes of HCV infection, the McKeating’s group developed a single-cycle co-culture assay to monitor single-cycle infection events, and to compare the efficiency of cell-free and cell-to-cell infection (Brimacombe et al., 2011; Meredith et al., 2013). They found that for all the strains tested, cell-cell transmission could be detected within 1h of co-culture of producer and target cells, whereas HCV cell-free infection was markedly delayed. More interestingly, they observed the difference in the ability to spread through cell-to-cell and cell-free routes for different HCV genotypes. In their study, HCV J6/JFH1 displayed 10-times higher rate of infection via cell-cell transmission compared to that of cell-free transmission, whereas HCV SA13/JFH1 and HK6A/JFH1 strains showed comparable rates of infection through both routes (Meredith et al., 2013).
HCV entry into hepatocytes
Both HCV cell-free and cell-to-cell infections require at least four essential cellular entry factors, including scavenger receptor SRB1, tetraspanin CD81, tight junction molecules CLDN1 and OCLN (Pileri et al.,1998; Scarselli et al., 2002; Evans et al., 2007; Timpe et al., 2008; Ploss et al., 2009; Brimacombe et al., 2011). Whether the exosome-mediated transmission also relies on these cellular factors remains unknown. HCV entry is a complex multiple-step event involving a number of cellular factors. Entry is initiated by the attachment of viral particles at the surface of host cells. Heparan sulfate proteoglycans (HSPGs) and low density lipoprotein receptor (LDLR) were indicated as the initial attachment factors interacting with HCV particles (Agnelle et al., 1999; Monazahian et al., 1999; Germi et al., 2002; Barth et al., 2003). (Fig.18 step1). After attachment, specific interactions between HCV envelope protein E2 and cellular factors SRB1 and CD81 are essential for the following steps of HCV entry involving other entry factors like the tight junction proteins CLDN1 and OCLN (Bartosch et al., 2003b; Stamataki et al., 2008; Harris et al., 2008; Harris et al., 2010). (Fig.18 step2-3). Eventually, HCV particles enter hepatocytes via clathrin-mediated endocytosis (Blanchard et al., 2006) (Fig.18 step4). Low pH environment in the early endosomes induces HCV fusion, leading to the uncoating of viral particle and delivering HCV genome RNA into the cytoplasm (Meertens et al., 2006). (Fig.18 step5). Newly identified host factors such as epidermal growth factor receptor (EGFR), ephrin receptor A2 (Lupberger et al., 2011). Niemann-Pick C1-like 1 (NPC1L1) (Sainz et al., 2012) and transferrin receptor 1 (TfR1) (Martin et al., 2013) have also been described to be involved in the entry process of HCV. Furthermore, receptor tyrosine kinases (RTKs) like EGFR have been demonstrated to be involved in HCV entry by regulating CD81-CLDN1 co-receptor associations (Lupberger et al., 2011). The GTPase HRas was found to act as a critical host signal transducer required for the lateral membrane trafficking of CD81, which enables the assembly of tetraspanin receptor complexes (Zona et al., 2013).
HCV envelope glycoproteins in viral entry
HCV envelope glycoproteins E1E2 by being present on the surface of viral particle are the major players in viral entry, and also are the primary targets of anti-HCV neutralizing antibodies. Functional E1E2 form a non-covalent heterodimer (Fig.18a), which is essential for HCV infectivity (Michalak et al., 1997; Bartosch et al., 2003b; Hsu et al., 2003; Op De Beeck et al., 2004). E1 and E2 are known to mediate the interactions with HCV cellular receptors/co-receptors, and also the fusion between the viral envelope and cell membranes following HCV internalization. The role of E1 in the entry process of HCV is not very clear yet, though it has been proposed to assist the fusion process (Lavillet et al., 2007) and a recent study suggested its role as a modulator for HCV binding to receptors and membrane fusion (Douam et al., 2013). By contrast, a large body of studies have been focused on the glycoprotein E2. Using its soluble form, researchers identified the first (CD81) and the second co-receptors (SRB1) required for HCV infection (Pileri et al., 1998; Scarselli et al., 2002). The positions of functional domains in E2 which mediate receptor binding are shown in Fig.18b. There exist at least two CD81-binding sites located at discrete regions (amino acids 412-443 and 520-550) in E2 (Flint et al.,1999a). The hypervariable region 1 (HVR1) has been proposed to be responsible for the interaction of E2 with GAGs and SRB1 (Barth et al., 2003; Scarselli et al., 2002). Two regions in E2 (amino acids 416-430 and 600-620) have been mapped as contributing to the fusion process (Lavillet et al., 2007). In the past years, as no crystal structure of E2 was available, and based on the comparison to other Flaviviruses and the distribution of its disulfide bonds, E2 was predicted to be a class II fusion protein with three domains (Krey et al., 2010). Recently, the core of E2 protein was successfully crystallized, however, the x-ray and electron microscopy showed that E2 structure differs remarkably from the former predictions (Kong et al., 2013; Khan et al., 2014).
Table of contents :
RÉSUMÉ
RÉSUMÉ
LONG
ABSTRACT
LIST OF ILLUSTRATIONS
LIST OF TABLES
ABBREVIATIONS
INTRODUCTION
I. GENERAL INTRODUCTION OF VIRAL HEPATITIS C
1. HEPATITIS C EPIDEMIOLOGY
2. NATURAL HISTORY OF HCV INFECTION
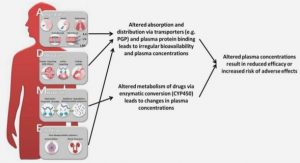
3. DIAGNOSIS AND TREATMENT OF HCV INFECTION
4. MOLECULAR BIOLOGY OF HCV
4.1 HCV classification and genotype distribution
4.2 HCV genome and viral proteins
4.3 The HCV life cycle
4.4 HCV particles
4.5 HCV model system
II. HCV VIRAL PARTICLE COMPONENTS IN VIRAL ENTRY
1. HCV HOST CELL TROPISM AND TRANSMISSION ROUTES
2. HCV ENTRY INTO HEPATOCYTES
3. HCV ENVELOPE GLYCOPROTEINS IN VIRAL ENTRY
4. HYPERVARIABLE REGION 1 OF ENVELOPE GLYCOPROTEIN E2
5. HCV PARTICLE COMPONENT APOE
5.1 ApoE protein and its isoforms in lipid metabolism and in AD
5.2 ApoE in infectious diseases
5.3 Influence of apoE isoforms in the HCV life cycle
6. OTHER APOLIPOPROTEINS
6.1 ApoCs in lipoprotein metabolism and HCV infection
6.2 ApoAI in lipoprotein metabolism and in HCV infection
III. CELLULAR FACTORS IN HCV ENTRY
1. HCV ATTACHMENT FACTORS
1.1 HSPGs
1.2 LDLr
2. HCV ENTRY RECEPTORS /CO-‐RECEPTORS
2.1 CD81
2.2 SRB1
2.3 Tight junction proteins
2.4 Other entry factors
3. THE INFLUENCE OF HCV INFECTION ON ITS ENTRY FACTORS
4. HCV ENTRY AS ANTIVIRAL TARGETS FOR THE DEVELOPMENT OF ANTI-‐HCV THERAPY
4.1 Targeting HCV envelope proteins
4.2 Targeting host factors involved in HCV entry
IV. HSPGS AND SYNDECAN FAMILY
1. SYNDECANS
2. HSPGS IN TRIGLYCERIDE-‐RICH LIPOPROTEIN (TRL) METABOLISM
3. HSPGS IN MICROBIAL INFECTIONS
4. BIOSYNTHESIS OF HEPARAN SULFATE (HS) CHAINS
5. HEPARIN AND HEPARIN OLIGOSACCHARIDES
OBJECTIVES
RESULTS
DISCUSSION&PERSPECTIVES
REFERENCES