Get Complete Project Material File(s) Now! »
Treatment of atherosclerosis: a brief history
While treatment of stable angina typically involves administration of medication and specific recommendations for lifestyle changes [22], lesions leading to unstable angina or even acute coronary syndrome require surgical intervention. In 1977 Andreas Grüntzig opened an entirely new chapter in the treatment of obstructed coronary arteries by inflating a catheter-mounted balloon at the site of the stenosis to re-open the artery [130]; percutaneous coronary inter-vention (PCI) was thus born. The great benefit of catheter-based balloon angioplasty (today referred to as « plain old balloon angioplasty » or POBA) for the patient was that the treatment was minimally invasive and did not require open heart surgery leading to significantly reduced recovery times.
Despite representing a major advance in cardiovascular intervention, POBA was not without its problems. In more than 50% of the cases this treatment failed due either to immediate vessel recoil or arterial restenosis (re-occlusion of the blood vessel due to uncontrolled growth of smooth muscle cells (SMCs) in reaction to the injury inflicted by the balloon). Another major advance was made in 1986 when Jacques Puel performed the first PCI on a human with a Palmaz-Schatz stent mounted on the balloon. The stent1, a tubular wire-mesh, remained in the artery after the intervention to serve as a permanent scaffold (Fig. 1.2). Although the use of a stent in PCI cut the rate of restenosis in half compared to POBA, restenosis remained a major complication in an unacceptably large fraction of the procedures. Restenosis occurs due to the uncontrolled proliferation of SMCs and their migration from the media into the intima (neointimal hyperplasia) and ultimately into the lumen where they form a new obstruction to blood flow. [157] was the development of drug-eluting stents (DES) which involve the addition of an anti-proliferative drug to the metallic bare-metal stent (BMS). The drug, most commonly sirolimus (or one of its derivatives) or paclitaxel, is released into the arterial wall where it inhibits SMC proliferation and hence prevents neointimal hyperplasia. With more than 7 million stent implantations per year worldwide (most of which are DES), the stent has become the most successful medical device for the treatment of advanced coronary atherosclerosis today. The drawback of using anti-proliferative drugs on stents is that these drugs also retard the healing process following the implantation process, mostly (but not exclusively) by delaying the recovery of the endothelium [54, 84, 85, 190]. Delayed endothelial recovery is associated with an elevated risk of late and very late stent thrombosis [53, 69, 84, 116, 131]. Stent thrombosis is the sudden formation of blood clots at the site of stent implantation. Depending on the time of occurrence relative to the intervention, stent thrombosis is classified in four types [170]: acute, within the first 24 hours; sub-acute, within the first 30 days; late, within the first year; and very late, after the first year. Whereas acute and sub-acute stent thrombosis are inherent to the foreign body response following implantation of stents (BMS or DES) [150], late and very late stent thrombosis Figure 1.2: Stenting procedure. A: A balloon-mounted stent is introduced to the site of the occlusive
atherosclerotic lesion via a catheter. B: The balloon is inflated at high pressure so that the ballon and stent compress the atherosclerotic plaque thereby re-opening the artery and restoring blood flow. C: The balloon is retracted and the stent remains as a permanent scaffold. Source: Encyclopædia Britannica Online. are far more likely to occur with DES than BMS. The unpredictability and high mortality of stent thrombosis make this complication, though rare, particularly serious. Addressing this complication requires extending the duration of an anti-thrombotic treatment in the aftermath of the surgery. The optimal duration of anti-thrombotic treatment remains, however, unknown. In light of these complications, questions have recently arisen on whether the scaffolding and drug elution characteristics of a stent are needed for longer than 6 months after the surgery. Proliferation of SMCs is significant for only the first few weeks [150], and complete remodeling of the arterial all is achieved within approximately 3 months [137]. In recent years, the above considerations have resulted in the development of biodegradable stents [61, 137] and in the revival of balloon angioplasty but now using balloons coated with an anti-proliferative drug, usually paclitaxel [66]. While both treatment options show very promising results, their long-term efficacy are yet to be established.
Anti-proliferative drugs: bliss and curse of drug-eluting stent design
A DES is comprised of three components: a stent body which provides the structural support, the drug to be eluted, and the drug carrier in which the drug is loaded and through which it is delivered. Each of these components has its own requirements [27, 101, 142]. The stent body needs to supply sufficient radial and axial strength, it needs to be very flexible to be easily deliverable even to the most complicated lesion, and the struts need to have a low profile to limit arterial damage at implantation and to minimize disturbance of the flow field in order to reduce the risk of thrombosis and facilitate re-endothelialization [33, 44, 96]. The geometry of the stent body also determines the release pattern for the drug into the arterial wall [11, 24, 51, 125, 127, 128, 162, 183, 201]. The drug carrier (typically a polymer) should be bio-compatible to prevent an inflammatory or rejection reaction. It should also enable controlled and sufficient release of drug, such that drug concentration in the arterial wall remains within the therapeutic window, i.e. sufficiently high to be effective and yet sufficiently low to avoid toxicity. The drug itself should effectively inhibit SMC proliferation within the first few weeks after the implantation [150] without causing secondary or long-term effects that compromise the integrity of the arterial wall. Finally, all of the stent’s components need to be finely tuned for the treatment to be successful both in the short and long terms.
How crucial stent design is to the success of a stenting procedure was emphasized by the results of the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) study [157] which demonstrated the superiority of second generation DES over both first generation DES and BMS. Second generation DES have undergone major design changes in their geometry, drug composition, and the composition of the drug carrier relative to the first generation devices [60]. Even among different second generation DES, significant differences in re-endothelialization outcomes have been observed with different stent designs [85, 132, 172].
The release kinetics of the drug from the drug carrier also play a crucial role for determining the therapeutic efficacy of a DES [7, 68, 102, 152, 165]. Moreover, the drug itself can be a design variable; interestingly, all drug-coated balloons currently under development use paclita-xel as the therapeutic agent of choice which is in contrast to developments in second generation DES, where manufacturers have for the most part opted for sirolimus (or its analogues) as the drug of choice.
Modeling drug transport in the arterial wall
The transport of an eluted drug within the arterial wall is governed by convection and diffusion through the tortuous pore space and to interactions with the cells of the arterial wall, most notably ECs and SMCs. If we want to understand and evaluate the therapeutic performance of DES, we need to first understand the processes occurring in the arterial wall, for which computational models would be particularly helpful. Consequently, significant scientific effort has been dedicated to study and model the transport of drugs [38, 81, 82, 105, 114, 179– 181] in the arterial wall, resulting in a variety of different modeling approaches ranging from relatively simple models that assume either a low drug diffusivity in the arterial wall [128] or a constant partition of bound and free drug [200] to more sophisticated models where drug interactions with the arterial wall are described by a second-order reversible reaction [24, 179]. With very few exceptions [51], these models approximate the arterial wall as a single homogeneous layer and often neglect convective drug transport within the wall.
Stent design optimization
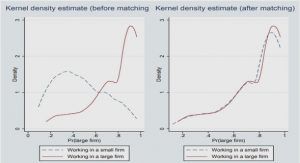
The broad variability in therapeutic success of DES in clinical use suggests that today’s DES designs are not necessarily optimal. Recognizing the shortcomings of today’s stents, pioneering studies of stent design optimization have been conducted over the past few years [9, 70, 71, 140, 141, 171]. These studies have so far been limited to optimizing geometrical features of stents. Modeling the physiologically relevant phenomena associated with stenting leads to complex computational models (see Chapter 2, [24, 51, 139]) that are computationally expensive to evaluate. A very versatile optimization framework used in the case of expensive computational simulations is the surrogate management framework (SMF) [23], since the use of classical optimization methods is often rendered infeasible. The SMF algorithm is a derivative-free optimization method which explores the space of possible designs by repeatedly evaluating the computational model for different sets of design variables. The algorithm uses a succession of search and poll steps to identify a set of design variables that yields the most optimal design. This method has previously been applied to the optimization of various aerospace [118, 119] and bioengineering [120, 198] systems.
Scope and outline of the present dissertation: optimization of drug-eluting stents
The present dissertation applies computational modeling to derive guidelines for novel stent designs that optimize DES performance. Recovery of the endothelium is particularly important for the success of a DES. Thus, we will focus our attention on the phenomena that appear to have a crucial impact on the endothelium: transport of the anti-proliferative drug eluted from the stent drug carrier and disturbance of the flow field due to the geometric design of the stent. In this work we will try to answer the following questions: What is an optimal stent? What design elements are crucial for obtaining an optimal stent? What should these design elements look like for an optimal stent? What is the role of the choice of drug in the optimization? We propose the following strategy to answer these questions: 1) We develop a computa-tional model of fluid flow and drug transport in stented arteries which serves to evaluate the performance of DES design. 2) We formulate a metric that quantifies DES performance. 3) We use a derivative-free optimization algorithm to minimize the cost function derived from the metric and hence identify optimal DES designs. In Chapter 2 we develop a computational model of drug transport that takes into account the multi-layered structure of the arterial wall, includes both convective and diffusive transport in the arterial wall, and incorporates a reversible binding model to describe drug interactions with the cells of the arterial wall [179]. The computational model is applied to study the transport dynamics of the two hydrophobic drugs paclitaxel and sirolimus. The sensitivity of the model predictions to several modeling parameters is also presented. The results of the simulations indicate a strong coupling between the drug dynamics in the arterial wall and the release kinetics of the drug from the stent drug carrier. This finding motivates the optimization of the drug delivery strategy, which we perform in Chapter 3. In Chapter 3 we introduce a cost function that serves as a quantitative measure of DES performance that assesses how well the applied drug delivery strategy maintains efficacious but sub-toxic drug concentration in the media while simultaneously minimizing drug concentration at the endothelial surface to facilitate re-endothelialization. We then minimize this cost func-tion by coupling a novel SMF optimization algorithm [16, 17] with our physiologically-based computational model derived in the previous chapter. Applying this approach, we identify the different drug delivery strategies that are needed for paclitaxel and sirolimus to yield optimal DES performance. Once drug delivery is optimized, Chapter 4 moves on to optimize DES strut shape. To this end, we extend our cost function to include a measure of the flow disturbance caused by the stent geometry. The particular SMF algorithm used here, which to our knowledge has never before been applied to engineering optimization, is particularly well suited to perform these more complex optimizations due to its regular and dense discretization of the design space and its novel poll step procedure. An analysis of the sensitivity of our cost function motivates the refinement of the optimization of the DES drug delivery strategies. The results of our investigation demonstrate that, to achieve optimal DES performance, strut shape and drug delivery need to be tailored to the drug dynamics in the arterial wall. The concluding remarks at the end of the dissertation contain a comprehensive summary of the results of all three chapters and make specific recommendations for future investigations.
Table of contents :
Contents
Abstract
Résumé
Acknowledgments
List of Figures
List of Tables
Nomenclature
1 Introduction
1.1 Atherosclerosis: a human condition?
1.2 Treatment of atherosclerosis: a brief history
1.3 Anti-proliferative drugs: bliss and curse of drug-eluting stent design
1.4 Modeling drug transport in the arterial wall
1.5 Stent design optimization
1.6 Scope and outline of the present dissertation
2 Modeling the Transport of Drugs Eluted from Stents
2.1 Introduction
2.2 Materials and methods
2.2.1 Model geometry
2.2.2 Physical model
2.2.3 Governing equations and boundary conditions
2.2.4 Determination of physiological parameters
2.2.5 Numerical methods
2.3 Results
2.3.1 Baseline model
2.3.2 Sensitivity analysis of the model
2.3.3 Effect of one-layer modeling
2.3.4 Effect of reaction modeling
2.3.5 Effect of the choice of drug
2.4 Discussion
2.4.1 Drug release is coupled to the drug and its transport properties in the arterial wall
2.4.2 Multi-layer model offers improved accuracy for pathological situations .
2.4.3 Reduction of the reaction model fails to capture important features of the transport dynamics
3 Optimized Drug Delivery for Drug-Eluting Stents
3.1 Introduction
3.2 Materials and methods
3.2.1 Computational model
3.2.2 Cost function
3.2.3 Optimization framework
3.2.4 Optimization cases
3.3 Results
3.3.1 Paclitaxel delivery optimization
3.3.2 Sirolimus delivery optimization
3.4 Discussion
3.4.1 Paclitaxel-eluting stents require quasi-bolus or zero-order drug release kinetics to avoid adverse concentration levels at the endothelium
3.4.2 Sirolimus-eluting stents require zero-order release kinetics due to sirolimus’ weak retention capabilities
3.4.3 Low-dose P-DES and S-DES with zero-order release kinetics lead to a similar shape of the cost function
3.4.4 The cost function responds to drug kinetics in the arterial wall
3.4.5 Paclitaxel vs. sirolimus: a settled debate?
4 Optimizing the Strut Design of Paclitaxel- and Sirolimus-Eluting Stents
4.1 Introduction
4.2 Materials and methods
4.2.1 Computational model
4.2.2 Cost function
4.2.3 Optimization method
4.2.4 Sensitivity estimation of the cost function to design variables and model parameters
4.3 Results
4.3.1 Sensitivity estimation of the cost function
4.3.2 Optimization results
4.4 Discussion
4.4.1 Optimal DES strut designs are tailored to optimized transport dynamics in the arterial wall
4.4.2 Optimal two-layered DES polymer coatings are tailored to the eluted drug
4.4.3 Challenges of the FDI weight factor
5 Conclusions
5.1 Future work
5.1.1 Additional physiological considerations
5.1.2 Expanding the cost function
5.1.3 Improved representation of the arterial wall
A Appendix
A.1 From the Brinkman equation to Darcy’s Law
A.2 Derivation of the weighted concentration
A.3 Including reaction at the endothelial surface
A.4 Governing equation for the equilibrium case
A.5 Remaining drug-dependent parameters of the model
A.6 Diffusivity of sirolimus
Bibliography