Get Complete Project Material File(s) Now! »
Development of inhibitory antibodies to therapeutic factor VIII in severe hemophilia A is associated with microsatellite polymorphism in the HMOX1 promoter
As described in section I.3.2.3, several SNPs in immune-related genes have been associated with the development of FVIII inhibitors in patients with severe hemophilia A.
Previous experimental observations from the lab have demonstrated that the administration of hemin to FVIII-deficient mice leads to the systemic induction of the heme-degrading enzyme, heme oxygenase-1 (HO-1), and was drastically reducing the anti-FVIII immune response (Dimitrov et al., 2010). In normal conditions, heme-bound hemoglobin is confined within erythrocytes, where it participates in the fixation and transport of oxygen. However, in the case of vascular damage, erythrocytes are lysed and their content is released in the micro-environment. Free heme, due to its redox properties, is potentially harmful in the sense that it can oxidize and damage any surrounding molecule. Thus, in response to heme exposure, several mechanisms are triggered, leading to the expression of HO-1. To date, three polymorphisms have been described in the HO-1 encoding gene (HMOX1), among which, two SNPs (-413 T>A and -1135 G>A) and one (GT)n repeat dinucleotide length polymorphism (Exner et al., 2004) (Figure 9). Although the nature of the SNPs does not seem to significantly modify the activity of the HMOX1 promoter, the length of the (GT)n repeats has been associated with the yield of expression of the HO-1 protein. From a mechanistic point of view, it is probable that the succession of (GT)n repeats confers a Z-conformation to the DNA, thus reducing the affinity for transcription factors. Thus, promoters with long (GT)n repeats would have less affinity for the transcription factors as compared to promoter with shorter (GT)n repeats.
Figure 9. HMOX1 promoter organization. The promoter region of the HO-1-encoding gene contains several transcription factor consensus binding sites, such as heat shock element (HSE), nuclear factor-κB (NFκB) and the activator protein-2 (AP-2). In addition to the (GT)n repeat dinucleotide length polymorphism (depicted in red), these additional transcription factor binding site possibly regulates the activity of the HMOX1 promoter.
The association between the number of (GT)n repeats has been associated with the outcome of various inflammatory conditions found in pulmonary, cardiovascular and autoimmune diseases. Results from these studies either associates long (GT)n repeats with a unfavourable outcome or short (GT)n repeats with a favourable outcome in these diseases (Exner et al., 2004).
Here, we wondered whether polymorphisms in the promoter of the HMOX1 gene could be associated with the development of FVIII inhibitors in patients with severe hemophilia A. Using a multi-centric cohort including 99 inhibitor-positive patients and 263 patients who did not develop inhibitors within the first 150 cumulative days of exposure to therapeutic FVIII, we demonstrated that patients with inhibitors have a higher frequency of alleles with large (GT)n repeats (L: n≥30) compared to patients without inhibitors (19.2% vs 9.3% respectively) and that genotypes containing the L allele were more frequent in patients with an inhibitor (odd ratio 2.31; 95% CI 1.46-3.66; P<0.001).
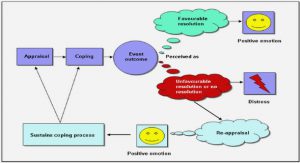
In this work, we demonstrated for the first time an association between a polymorphism in the promoter of the stress-inducible HMOX1 gene with the risk of developing FVIII inhibitors. Moreover, these results suggest that the capacity of the patients to cope with inflammation, associated or not with hemorrhages may be a critical parameter influencing the initiation of the anti-FVIII immune response.
As presented in section I.3.2.3, a recent GWAS analysis was conducted using a combined cohort involving 833 patients with severe hemophilia A from three independent cohorts (HIGS, MIBS and HGDS). This GWAS analysis, including 13,331 SNPs from 1,081 genes, resulted in the identification of 53 SNPs as significant predictors of inhibitor status. The 5 SNPs that were concordant in the three cohorts and are associated with a higher risk for the development of inhibitors have odd ratios as high as 4.29. However, GWAS analyses focus only on SNPs, and do not include length polymorphism, thus explaining why the number of (GT)n repeats in the promoter of the HMOX1 gene was not identified in the GWAS analysis conducted by Prof Astermark. In contrast to the GWAS strategy, which screens thousands of genes, our approach was candidate-gene driven, based on the experimental finding that induction of HO-1 in mice had a protective effect on the development of FVIII inhibitors. While having two opposite starting points, these two strategies are complementary in the identification of the patient‟s genetic profiles associated with higher risks for the development of FVIII inhibitors.
Hemarthrosis and arthropathies do not favor the development of factor VIII inhibitors in hemophilia A mice
As described in section I.1.1.4, the lack of functional endogenous FVIII in patients with severe hemophilia A leads to the development of hemarthrosis and ensuing arthropathies. Beside the crippling effects of such complications, little is known about the participation of such events on the development of FVIII inhibitors. However, the presence of concomitant bleedings as a risk factor for the development of FVIII inhibitor has been suggested and is detailed in section I.3.3.3. Unlike humans, the mouse model for FVIII-deficiency does not have the same pathophysiological development. Indeed, FVIII-deficient mice do not present spontaneous bleedings, and do not develop arthropathies. However, the insertion of a needle below the patella of FVIII-deficient mice generates a localized hemarthrosis which is resorbed within 14 days, and leads to the development of knee arthropathy (Hakobyan et al., 2008). Thus, using an established model of knee puncture in FVIII-deficient mice, we asked the question of the development of FVIII inhibitors in this particular situation To follow the anti-FVIII immune response in the mouse model of hemarthrosis or arthropathy, FVIII replacement therapy was initiated 1, 7 or 14 days after puncture of the knee. Anti-FVIII IgG titres and inhibitory titres were determined in the serum of mice by ELISA and Bethesda assay three days after the second, third and fourth injection of therapeutic FVIII. The results obtained from these experiments demonstrate that the presence of hemarthrosis or arthropathies do not represent a risk factor for the anti-FVIII immune response, as the anti-FVIII IgG titres were not increased in mice with hemarthrosis and arthropathies compared to un-injured mice. Conversely, we observed a significant reduction of the anti-FVIII IgG titres in mice where the FVIII replacement therapy was initiated 7 days after knee injury. Because of the presence of blood at the site of injury, and after having ruled out an increased consumption of FVIII, we assessed the induction of HO-1 in these mice by western-blot.
Indeed, systemic induction of HO-1 in mice drastically reduces the anti-FVIII immune response (Dimitrov et al., 2010). We found that HO-1 was induced 7 days after puncture of the knee, and was concomitant with the reduction in the anti-FVIII immune response. Moreover, we analysed the expression of maturation markers in the splenic antigen presenting cells by flow cytometry. We observed that 7 days after puncture of the knee of FVIII-deficient mice, the level of expression of MHC class II and CD86 were significantly reduced in dendritic cells and macrophages. Taken together, our results demonstrate that bleedings in FVIII-deficient mice do not represent a danger signal that adjuvant the anti-FVIII immune response.
Our observations are important in view of the fact that bleeding, surgery and vaccination have often been proposed as risk factors for the development of FVIII inhibitors. Importantly, no scientific demonstration has been provided in favour of any of these factors. Potential limitations of the present work reside in the use of the mouse model of severe hemophilia A. Indeed, in contrast to patients in whom the severe hemophilia A phenotype may be due to different types of mutation, with all the possible consequences on the ontogeny of the immune system as described in section I.1.1.3, the mouse model of hemophilia A is completely naïve for the human FVIII molecule. The identification of the risk factors for the development of FVIII inhibitors is complicated by the fact that administration of FVIII in FVIII-deficient mice systematically triggers an anti-FVIII immune response. Accordingly, due to the congenic nature of the FVIII-deficient mice strain, their ability to turn on the anti-inflammatory machinery upon bleeding is probably similar in every individual, and do not reflect the heterogeneity that is the hallmark of the human situation, as highlighted in section II.1.
Restoration of the oxidative balance in factor VIII-deficient mice reduces the immunogenicity of therapeutic factor VIII
As described in section I.3.3.3, a pro-inflammatory state of the immune system at the time of FVIII administration is considered as a risk factor facilitating the development of FVIII inhibitors. Thus, bleedings are associated with the triggering of the respiratory burst in innate immune cells that are recruited at the site of injury. The respiratory burst leads to the generation of reactive oxygen species (ROS) the primary function of which is to destroy potentially invading pathogens. However, ROS are not specific to pathogens and will act non-specifically on any molecule present in the surrounding environment. Thus, excessive accumulation of ROS has a deleterious effect and may lead to damages to self-proteins. To counteract these undesirable effects of excessive ROS accumulation, several enzymatic and non-enzymatic antioxidant systems have evolved.
In this work, we hypothesized that the lack of functional endogenous FVIII in FVIII-deficient mice is associated with an increase ROS accumulation. Because the quantification of ROS is complicated by their short half-life, we aimed at determining the status of the endogenous antioxidant systems, as an indirect proof of chronic ROS generation. Thus, we compared the oxidant radical absorbance capacity (ORAC) of plasma from FVIII-deficient mice to that of wild-type C57Bl/6 mice. We found that plasma from FVIII-deficient mice has lower ORAC value compared to that of C57Bl/6 mice (2511±32 vs 2666±44 Trolox equivalent, P<0.05). This observation was confirmed using the ferric reducing ability of plasma (FRAP) assay.
We then hypothesized that the supplementation of mice with the antioxidant N-acetyl-L-cysteine (NAC) would restore the redox balance and will affect the anti-FVIII immune response. Thus, NAC (0.142g/L) was added to the drinking water of mice throughout the FVIII-immunization protocol. We validated that the supplementation with NAC was restoring the ORAC value of the plasma of FVIII-deficient mice. Moreover, we found that mice treated with NAC had lower anti-FVIII IgG titres compared to that of untreated mice (675.0±129.3 vs 358.5±74.3, P < 0.05). Importantly, the treatment of mice with NAC was not impairing the ability of their immune system to mount an immune response, as the total IgG titres and the immune response to tetanus toxin were equal in both NAC-treated and control group.
Taken together, these results demonstrate that the lack of FVIII in FVIII-deficient mice is associated with a reduced capacity of the plasma to scavenge ROS. This might be due to a chronic generation of ROS that might originate from chronic bleedings, despite the absence of overt hemorrhages. These identify the redox state as a risk factor for the development of the anti-FVIII immune response. However, these data were obtained using the FVIII-deficient mouse model. It would be interesting to determine whether these results are reproducible in patients with hemophilia A. If so, the determination of the redox state in patient might be seen as a predictive tool for the development of inhibitors. Moreover, the use of antioxidant compounds might lower the risk of patients with hemophilia A to develop FVIII inhibitors.
Oxidation of therapeutic factor VIII aggravates its immunogenicity in factor-VIII deficient mic Manuscript in preparation (discussion pending, but results are discussed in chapter III)
The occurrence of cellular damage triggers the inflammatory machinery. A major arm of the inflammatory machinery resides in the recruitment and activation of phagocytic cells at the damaged site. The role of activated phagocytes at the site of injury is to limit the invasion of pathogens. To achieve this goal, phagocytes dispose of a wide arsenal to directly destroy pathogens, or to facilitate their neutralization by the other components of the immune system. Indeed, in 1973, Babior et al. reported that phagocytes utilize a membrane-bound NADPH oxidase to generate large amounts of reactive oxygen species (ROS) (Babior et al., 1973). The process of ROS generation and secretion is described as the “respiratory burst” or “oxidative burst”. This system comprises a wide variety of mediators acting on several types of molecules.
From a chemical point of view, the membrane-bound NADPH oxidase generates a superoxide anion (O2●-), which is then dismuted to H2O2 and oxygen by the superoxide dismutase (SOD). Later on, H2O2 is converted into hypochlorous acid (HOCl). Although the generated ROS may directly destroy the target antigens, they also exert multiple functions on the immune response, which can be direct, by affecting the signalling of immune cells, or indirect, through alterations of the antigens that are addressed to the immune system.
ROS react rapidly with the surrounding proteins, DNA or lipids. In the case of HOCl however, it seems that proteins are likely to be the main target. As a selective oxidant, HOCl reacts with particular amino acids. Thus, the order of reactivity for protein side chain is Met > Cys >> Cystine ~ His ~ α-amino > Trp > Lys >> Tyr > Arg > Gln ~ Asn (Pattison and Davies, 2001). Once the reactive side-chain residues have been consumed, and if the concentration of HOCl increases, the backbone amides of the protein are targeted by HOCl. The attack of the backbone amides by HOCl results in the fragmentation of the target protein. Thus, oxidative damages on a singular protein depend on the composition and the accessibility of the amino acids of the protein.
From an immunological point of view, the oxidative alteration of antigens has been repeatedly associated with a higher immunogenicity. In this work, we hypothesized that the oxidative modification of FVIII, which may occur at the site of bleeding, modulates its immunogenicity. As a model for ROS, we used hypochloric acid (HOCl), which is the most abundant ROS released by neutrophils. Our results demonstrate that exposure of FVIII to HOCl result in a dose-dependent loss of FVIII pro-coagulant activity. To characterize the impact of the exposure of FVIII to HOCl, we studied the association of native or HOCl-exposed FVIII to its natural binding partners. We found no major changes in the ability of HOCl-exposed FVIII to bind VWF, phosphatidyl serine, and four monoclonal antibodies (BO2C11, BO2BII, ESH8 and 77IP52H7). We demonstrate that the exposure of FVIII to a 25-fold molar excess of HOCl results in the disappearance of free amines without the generation of carbonyls groups. This suggests that the exposure of FVIII to a 25-fold molar excess of HOCl results in a mild oxidation of the FVIII molecule. In vivo, we demonstrate that, as hypothesized, exposure of FVIII to HOCl modulates FVIII immunogenicity. Indeed, FVIII-deficient mice treated with FVIII that was exposed to a 25-fold molar excess of HOCl, mounted a higher anti-FVIII immune response compared to mice treated with native FVIII. In an attempt to understand the underlying mechanism, we demonstrate that the exposure of FVIII to a 25-fold molar excess of HOCl does not inducing the maturation of human DCs in vitro. However, the incubation of splenocytes from FVIII-primed mice with HOCl-exposed FVIII resulted in a higher proliferation compared to that of splenocytes incubated with untreated FVIII.
Further work is required to complete our observations. Thus, the binding of FVIII or HOCl-exposed FVIII to FIXa has not been explored yet. Similarly, the endocytosis of HOCl-exposed FVIII has to be investigated, although a first set of experiment suggested no change in FVIII uptake following exposure to HOCl. Several studies suggest that the oxidative modification of antigens is associated with a modified susceptibility of the antigen to be processed in the endosome of antigen-presenting cells. Thus, we will compare the susceptibility of FVIII and HOCl-exposed FVIII to be cleaved by endosomal proteases (e.g. cathepsins).
Table of contents :
I. INTRODUCTION
I.1. Hemophilia A
I.1.1. Generalities
I.1.1.1. Historical aspects
I.1.1.2. Phenotypic aspects
I.1.1.3. Genetic aspects
I.1.1.4 Bleeding complications in Hemophilia A
I.1.2 The coagulation cascade
I.1.2.1 Primary haemostasis
I.1.2.2 Secondary haemostasis
I.1.2.2.1 The extrinsic pathway
I.1.2.2.2 The intrinsic pathway
I.2.2.3 Pro-coagulant factor VIII
I.2.2.3.1 Synthesis, structure and post-traductional modifications
I.2.2.3.2 Activation of FVIII
I.2.2.3.3 Life cycle of FVIII, catabolic receptors, in vivo distribution, site of elimination
I.2.2.3.4 Catabolic receptors for FVIII
I.2.2.3.5 In vivo distribution of FVIII
I.1.3 Prevention or treatment of bleeding episodes in patients with hemophilia A
I.1.3.1 Factor VIII products
I.1.3.2 Infusion regiment
I.1.3.3 Complications of the treatment
I.1.3.4 Treatment of patients with FVIII inhibitors
I.2 The anti-factor VIII immune response
I.2.1 FVIII as seen by the immune system in patients with hemophilia A
I.2.2 Antigen-presenting cells
I.2.2.1 Dendritic cells
I.2.2.2 Macrophages
I.2.2.3 B cells
I.2.3 The spleen
I.2.4 The anti-FVIII immune response in hemophilia A patients
I.2.4.1 T-cell activation
I.2.4.2 B-cell activation
I.3 Risk factors
I.3.1 The danger signal theory
I.3.1.1 Exogenous danger signals
I.3.1.2 Endogenous danger signals
I.3.2 Genetic risk factors
I.3.2.1 FVIII mutations
I.3.2.2 HLA haplotype
I.3.2.3 Polymorphisms in immune-related genes
I.3.3 Non-genetic risk factors
I.3.3.1 Age at the start of treatment
I.3.3.2 Mode and intensity of FVIII administration
I.3.3.3 State of the immune system at the time of FVIII infusion
I.4 Purpose of the PhD work
II. RESULTS
II.1. Development of inhibitory antibodies to therapeutic factor VIII in severe hemophilia A is associated with microsatellite polymorphism in the HMOX1 promoter
II.2. Hemarthrosis and arthropathies do not favor the development of factor VIII inhibitors in hemophilia A mice
II.3. Restoration of the oxidative balance in factor VIII-deficient mice reduces the immunogenicity of therapeutic factor VIII
II.4. Oxidation of therapeutic factor VIII aggravates its immunogenicity in factor-VIII deficient mice
III. DISCUSSION
IV. REFERENCES
V. ANNEXES