Get Complete Project Material File(s) Now! »
Discovery of hepatitis C virus
In the early seventies, the only viruses known to be responsible for transfusion-associated hepatitis were hepatitis A virus (HAV) (Bayer et al., 1968) and hepatitis B virus (HBV) (Feinstone et al., 1975) for which serological tests were available. Hepatitis A and hepatitis B diseases differ in their mode of transmission and symptoms. Hepatitis A is transmitted by person to person contact or through consumption of contaminated food or water, characterized by a short incubation time (1-3 weeks) and results in an acute serious sickness but does not lead to chronic hepatitis. While hepatitis B is transmitted through blood or body fluid, has a longer incubation period (1-3 months) and causes a chronic infection (Krugman et al., 1967). However, at that time, it was discovered that an important number of post-transfusion hepatitis was not due to infection by HAV and HBV, suggesting the existence of a yet unknown hepatitis virus (Alter et al., 1975; Feinstone et al., 1975). As a consequence, these hepatitis were called the non-A non-B hepatitis (NANBH). In 1989, the identification of the hepatitis C virus could be achieved by screening a cDNA library obtained from a highly infectious chimpanzee plasma with antibodies from infected patient sera (Choo et al., 1989). Further experimentation revealed that the infectious agent was a small enveloped virus carrying a single-stranded RNA (ssRNA) genome of ~ 10 kb with a single open reading frame (ORF). The new virus was named hepatitis C virus (HCV) and was classified in the genus hepacivirus of the Flaviviridae family (Choo et al., 1989). This discovery allowed for the development of HCV diagnosis tests, which led to a great decrease of the risk of infection by the virus.
HCV classification and genetic variability
HCV belongs to the hepacivirus genus in the Flaviviridae family (Fig.1) which comprises 3 further genera: the flaviviruses (e.g. dengue virus), pestiviruses (e.g. bovine viral diarrhoea virus) and pegiviruses (e.g.GB viruses) (Simmonds et al., 2017). Members of the Flaviviridae family share similarities in terms of virion morphology, genome organization and replication strategy. Until recently, there was no evidence for the existence of HCV animal homologs. In 2011, however, the first evidence for a wider hepaciviral host range emerged, with the isolation of a novel hepacivirus species in dogs and horses (Burbelo et al., 2012; Kapoor et al., 2011; Pfaender et al., 2015; Ramsay et al., 2015). Since then, HCV homologs were isolated in bats, rodents, primates, bovines and sharks (Hartlage et al., 2016). Thus, the identification of animal hepaciviruses contributes to increase our understanding of hepacivirus origin and their host range determinants.
HCV epidemiology
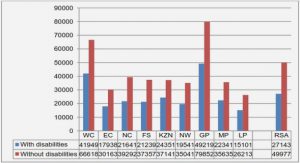
HCV has been reported to infect more than 170 million people around the world, which corresponds to 3% of the global population (Mohd Hanafiah et al., 2013). These figures were based on testing seroprevalance of antibodies to HCV in the population. Nevertheless, the presence of anti-HCV antibodies in the serum constitutes evidence of past or present HCV infection. Eventually, recent figures of HCV global prevalence based on HCV RNA positivity show lower prevalence, with around 71 million HCV infected individuals in 2015 (The Polaris Observatory HCV Collaborators, 2017). HCV prevalence varies among countries around the world (Fig.3). High prevalence of HCV infection can be attributed in some countries to the use of contaminated medical devices and equipment. One example is Egypt, which has a high seroprevalence of > 10% and is considered to have the highest HCV prevalence worldwilde. This could be traced back to anti-schistosomiasis (flat worms) campaigns between the 1960s and 1980s (Strickland, 2006; Arafa et al., 2005; Frank et al., 2000), during which, contaminated needles and syringes might have been re-used. In addition to Egypt, other developing countries like Cameroon, Gabon, Georgia, Pakistan, Mongolia and Uzbekistan (Baatarkhuu et al., 2017; Karchava et al., 2015; Nerrienet et al., 2005; Njouom et al., 2012; Ruzibakiev et al., 2001) are reported to have >5% of anti-HCV antibody prevalence, where iatrogenic infection (infections transmitted during medical treatment and care) plays the main role for infection in these countries. Variously, in western countries as North America and Western Europe only a low percentage of HCV global prevalence (< 2%) exists and the main risk factor for HCV infection is the unsafe injection drug use (Gower et al., 2014).
HCV Pathogenesis
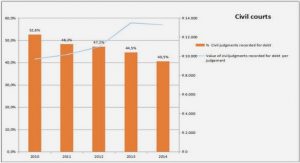
Hepatitis C is a long-lasting disease that evolves slowly. The first phase of hepatitis C consists in an acute infection that is in most cases asymptomatic. In 80% of the cases, patients develop a chronic infection that can lead in 20% of the cases, to cirrhosis and ultimately to hepatocellular carcinoma over a 20 years period (Fig.4) (Freeman et al., 2001; Stanaway et al., 2016). Importantly, hepatitis C is the major cause for liver transplantation in many parts of the world (Gower et al., 2014).
Table of contents :
ABSTRACT
RESUME
LIST OF FIGURES AND TABLES
ABBREVIATIONS
1 INTRODUCTION
1.1 HEPATITIS C VIRUS: AN OVERVIEW
1.1.1 Hepatitis
1.1.2 Discovery of hepatitis C virus
1.1.3 HCV classification and genetic variability
1.1.4 HCV transmission
1.1.5 HCV epidemiology
1.1.6 HCV Pathogenesis
1.1.6.1 Acute hepatitis
1.1.6.2 Chronic hepatitis
1.1.7 Immunology
1.1.7.1 Innate Immunity
1.1.7.2 Adaptive Immunity
1.1.7.2.1 Humoral immune response
1.1.7.2.2 Cell mediated immune response
1.1.8 Diagnosis of HCV
1.1.8.1 Serologic Assays
1.1.8.2 Molecular Assays
1.1.8.3 HCV genotyping
1.1.9 Treatment of HCV infection
1.1.9.1 Current Treatment
1.1.9.2 HCV vaccine
1.2 HCV VIRAL STRUCTURE AND FUNCTION
1.2.1 HCV viral particle
1.2.2 HCV genome organization and function
1.2.2.1 The 5’UTR
1.2.2.2 The 3’UTR
1.2.2.3 Core
1.2.2.4 HCV envelope glycoproteins E1E2
1.2.2.5 p7 protein
1.2.2.6 NS2 protein
1.2.2.7 NS3 and NS4A
1.2.2.8 NS4B
1.2.2.9 NS5A
1.2.2.10 NS5B
1.3 MODELS FOR THE STUDY OF HCV
1.3.1 The HCV replicon system
1.3.2 HCV pseudoparticles
1.3.3 HCVcc culture system
1.3.3.1 HCVcc
1.3.3.2 HCV Permissive cell lines
1.3.4 HCV Animal models
1.3.4.1 Chimpanzee
1.3.4.2 Genetically humanized mouse models
1.3.4.3 Human liver-chimeric mice
1.3.4.4 HCV homologs
1.4 HCV LIFE CYCLE
1.4.1 HCV entry
1.4.1.1 Attachment factor
1.4.1.1.1 Glycosaminoglycans
1.4.1.1.2 Lectins: DC-SIGN/L-SIGN
1.4.1.1.3 Low Density Lipoprotein Receptors
1.4.1.2 HCV-specific receptors
1.4.1.2.1 CD81 tetraspanin
1.4.1.2.2 SRBI
1.4.1.2.3 CLDN1
1.4.1.2.4 OCLN
1.4.1.3 Fusion of viral and host membranes
1.4.1.4 Mechanism of HCV entry
1.4.1.5 Cell-to-cell transmission
1.4.2 HCV translation
1.4.3 HCV replication
1.4.4 HCV assembly
1.5 HCV GLYCOPROTEINS E1 AND E2
1.5.1 E1 and E2 biogenesis
1.5.1.1 E1E2 heterodimer formation
1.5.1.2 Folding, glycosylation and disulphide bonds formation
1.5.2 E2 glycoprotein
1.5.2.1 E2 structural organization
1.5.2.2 E2 Neutralization
1.5.2.3 Role of E2 in attachment and binding
1.5.3 E1 glycoprotein
2 AIMS OF THE STUDY:
3 RESULTS:
4 DISCUSSION:
5 MATERIALS AND METHODS:
5.1 CLONING OF VIRAL MUTANTS
5.2 RNA INTERFERENCE EXPERIMENTS
5.3 VIRAL RNA QUANTIFICATION AND VIRUS PRECIPITAION BY POLYETHYLENE GLYCOL (PEG)
ANNEX:
6 REFERENCES: